Second Draft Statement on the Safety of Ginger Supplement Use in Pregnancy
Introduction - Second Draft Statement on the Safety of Ginger Supplement use in Pregnancy
In this guide
In this guideThis is a paper for discussion.
This does not represent the views of the Committee and should not be cited.
1. As part of the current programme of work on the maternal diet, the Committee considered the use of dietary supplements during pregnancy. A scoping paper (TOX/2020/51) was presented, reviewing the commonly used dietary supplements during pregnancy. These were supplements that were not officially recommended by the relevant authorities, but which were promoted by anecdotal evidence and unofficial sources as having various purported benefits. The review was confined to herbal dietary supplements which would be regulated under food law, and which would not be considered to be traditional herbal medicines which are the responsibility of the Medicines and Healthcare Products Regulatory Agency (MHRA). Following this review, the COT agreed ginger required further investigation, noting that human, animal and in vitro data were available.
2. In May 2021, the Committee considered the potential effects of ginger and ginger supplements during pregnancy and lactation. Paper TOX/2021/26 (Available on the COT website) reviewed the available data on toxicity to the mother, effects on the development of the fetus or embryo, and possible interactions with drugs as well as data on potential exposure.
3. Overall, it was concluded that there were limited data. The human data presented were not strongly indicative of any toxicological concern but there were some indications of possible adverse effects and a lot of uncertainties. Ginger did not appear to be systemically toxic but did appear to have reprotoxic effects at high supplemental doses. The Committee suggested looking at the animal data in closer detail to determine the point of departure (No Observed Adverse Effect Level - NOAEL), followed by calculating the potential exposure to supplements to determine whether there was cause for concern.
4. Paper TOX/2021/51 provided further information with respect to animal studies, contaminants and exposure to ginger supplements, primarily centred on the effect of ginger on prostaglandins, reproductive and developmental toxicity and the possible contaminants present in ginger.
5. The members noted that although the different ginger extracts were not comparable, they did appear to exhibit some biological activity in the early stages of pregnancy. It was reiterated that there was no indication of general systemic toxicity from the use of ginger.
6. A draft statement was considered in July 2022 (TOX/2022/42), drawing on the information provided in the previous discussion papers to form an overall conclusion on the safety of the use of ginger and in particular ginger supplements in the maternal diet.
7. The current statement includes additional studies identified by the COT to further inform the available database, with regard to the possible influence of ginger components on cyclooxygenase (COX) and prostaglandin activity. A summary of all the studies considered has also been tabulated in Annex B for reference.
Questions for the Committee
i. Does the additional information provided change the final conclusion of the statement?
ii. Does the committee have any further comments on the content and structure of this statement?
Secretariat
December 2023
Annex A - Second Draft Statement on the Safety of Ginger Supplement Use in Pregnancy
In this guide
In this guideBackground
1. As part of the current programme of work on the maternal diet, the Committee considered the use of dietary supplements during pregnancy. A scoping paper (TOX/2020/51) was presented, reviewing the commonly used dietary supplements during pregnancy. These were supplements that were not officially recommended by the relevant authorities, but which were promoted by anecdotal evidence and unofficial sources as having various purported benefits. The review was confined to herbal dietary supplements which would be regulated under food law, and which would not be considered to be traditional herbal medicines which are the responsibility of the Medicines and Healthcare Products Regulatory Agency (MHRA). Following this review, the COT agreed ginger required further investigation, noting that human, animal and in vitro data were available.
2. Paper TOX/2020/51 provided a detailed summary of the supplements most recommended during pregnancy (ginger, chamomile, raspberry leaf, echinacea, peppermint oil and leaves, dandelion, and evening primrose oil), focusing where available, on studies relevant to pregnancy and maternal outcomes. The main areas of investigation were general toxicity to the mother, effects on the development of the fetus or embryo, and possible interactions with medicines. Members suggested that ginger required further investigation, noting that both human and animal in vitro and in vivo data were available.
3. In May 2021, the Committee considered the potential effects of ginger and ginger supplements during pregnancy and lactation. Paper TOX/2021/26 (Available on the COT website) reviewed the available data on toxicity to the mother, effects on the development of the fetus or embryo, and possible interactions with drugs as well as data on potential exposure.
4. Overall, it was concluded that there were limited data. The human data presented were not strongly indicative of any toxicological concern but there were some indications of possible adverse effects and a lot of uncertainties. Ginger did not appear to be systemically toxic but did appear to have reprotoxic effects at high supplemental doses. The Committee suggested looking at the animal data in closer detail to determine the point of departure (No Observed Adverse Effect Level - NOAEL), followed by calculating the potential exposure to supplements to determine whether there was cause for concern.
5. Paper TOX/2021/51 provided further information with respect to animal studies, contaminants and exposure to ginger supplements, primarily centred on the effect of ginger on prostaglandins, reproductive and developmental toxicity and the possible contaminants present in ginger.
6. The members noted that although the different ginger extracts were not comparable, from animal studies they did appear to exhibit some biological activity in the early stages of pregnancy. It was reiterated that there was no indication of general systemic toxicity from the use of ginger.
7. Initially, the COT noted that intake of ginger in foodstuffs should also be considered as ginger was noted to be consumed not only as a supplement but also as part of the diet in foods such as ginger biscuits, tea and ginger beer. Therefore, aggregate exposures would need to be considered when addressing the safety of ginger supplement use during pregnancy.
Annex A - Information on ginger
In this guide
In this guide8. Ginger (Zingiber officinale) is a flowering tropical plant originating in Southeast Asia and grown in warm climates including China, India, Africa and the Caribbean. Ginger is commonly consumed in fresh root, dried root powder and capsule (encapsulated dried powder) forms, as a liquid extract, preserved in syrup or sugar and as a tea.
Uses
9. The rhizome (underground stem) of the ginger plant is commonly used as a spice and flavouring in many countries around the world and is increasingly growing in popularity as a natural remedy due to its purported immune system-boosting properties and also to alleviate motion sickness and post-operative nausea and vomiting. Ginger has been recommended for the treatment of pregnancy-related nausea (NHS 2021; NICE 2021) and has also been used as a dietary supplement and a traditional remedy in many cultures. Ginger is included in the official pharmacopoeias of some western countries.
Constituents
10. Over 100 compounds have been identified in ginger extracts, the main being terpenoids - mainly sesquiterpenoids (α-zingiberene, β-sesquiphellandrene, β-bisabolene, α-farnesene, ar-curcumene (zingiberol) and smaller amounts of monoterpenoids (camphene, β-phellandrene, cineole, geraniol, curcumene, citral, terpineol, borneol) (EMA, 2012).
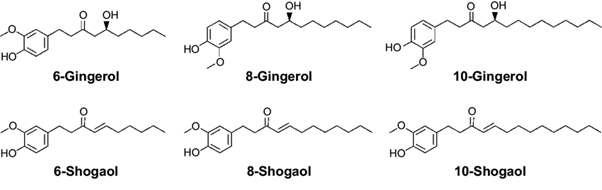
11. The ginger rhizome contains two main classes of constituents: the essential oils responsible for the aroma, and the main pungent principles, gingerols and shogaols. Organic acids are also present in smaller amounts. Depending on the area of cultivation, gingerols make up 4-7.5% of the pungent principles, the main one being 6-gingerol. Gingerols of other chain lengths are also present in smaller amounts.
Reviews by other regulatory agencies
12. Ginger is included in the official pharmacopoeias of several western countries. Ginger is classified as ‘Generally Recognised as Safe’ (GRAS) by the United States Food and Drug Administration (FDA) however, few specific studies have been carried out to evaluate the safety of ginger use during pregnancy and lactation. A report by the National Institute for Health and Care Excellence (NICE) cites a number of short duration trials which have been conducted in pregnant women (NICE, 2021).
13. In 2008, the Danish company Ferrosan A/S withdrew their product GraviFrisk – a product containing 6 g of dried ground ginger - from market, due to concerns surrounding the lack of safety data with respect to the use of supplements containing highly concentrated ginger extracts by pregnant women (Dietz et al., 2016).
14. In their 2012 report on ginger root in powdered form, the European Medicines Agency (EMA) concluded “The ginger extract dosages to provoke acute toxicity are high and much higher than usually administered dosages (factor 10-15 for an adult). There is some evidence that ginger root may cause testicular weight to increase by repeated high dosages of ginger root extract (2000 mg/kg). Ginger root has mutagenic as well as antimutagenic properties in microbial test systems. Developmental toxicity studies in rats are difficult to interpret, however, it is probably not a cause for concern. In general, toxicity studies of ginger are considered inadequate at least regarding genotoxicity, carcinogenicity and, partially, reproductive and developmental toxicity.”
15. The Norwegian Food Safety Authority have issued a warning regarding the use of ginger supplements and ginger-containing shots during pregnancy. This was based on a risk assessment carried out by the Danish Technical University and the Danish Veterinary and Food Administration (DTU, 2018). The assessment, based on animal studies, including one where rats were treated with a fresh grated ginger preparation with ginger at concentrations of 20-50 g/L in water, found that even in the 20 g/L treatment group – the equivalent of 1,784 mg/kg bw increased the incidence of abortion in rats. The Norwegian Food Safety Authority concluded that while a woman of 70 kg would consume less ginger (124 mg to 329 mg) there remains cause for concern and fetal risk cannot be excluded.
16. Recently, the Finnish Food Authority has issued a recommendation against the use of products containing ginger concentrate or extract, ginger tea and food supplements containing ginger by pregnant and breastfeeding women, infants and toddlers, schoolchildren, elderly and individuals with weakened immunity (Finnish Food Authority, 2019). It was noted that the concentrates contained harmful substances and safe consumption levels were unknown.
Health-based guidance values
17. There are currently no health-based guidance values (HBGV) with respect to ginger or its main components. Exposure to ginger was considered based on information found on supplement and tincture composition and background diet, but the variability of available supplements meant exposure also varied, which made comparison difficult.
18. The NHS and NICE recommend the use of ginger tea and biscuits for the treatment of nausea and vomiting in pregnancy (NHS, 2021; NICE, 2021). Generally, amounts of 1 g ginger per day have been recommended (NHS, 2022). Anecdotally, 1-1.5 g per day has also been advised during pregnancy (Healthline, 2020; Mother and baby, 2022). The use of supplements under the advice and supervision of a medical professional is advised.
Toxicology
19. It was noted that some studies detailed effects on male testes and, though not relevant for females, they were nevertheless regarded as indicating a potential reprotoxic effect from ginger. Studies suggest that ginger affected the viability of pregnancy; however, with no strong conclusive human data, the COT concluded that more work was required, especially as these studies suggested a link between first trimester loss and ginger use. Further, the possible fetotoxicity based on evidence from animal data, genotoxicity and possible drug interactions should be further investigated.
20. Discussion paper TOX/2021/26 reviewed the available studies on cytotoxicity, mutagenicity, acute, reproductive and developmental toxicity, lactation and possible drug interactions as well as data on potential exposure in pregnancy, covering both animal and human studies. The results from these reports were varied due to the differences in the forms and extracts tested and as a result, some findings were contradictory.
21. Paper TOX/2021/51 provided further information with respect to animal studies, contaminants and exposure to ginger supplements, primarily centred on the effect of ginger on prostaglandins, reproductive and developmental toxicity and the possible contaminants present in ginger. The Committee noted that the papers reviewed covered ginger in a range of forms including fresh, aqueous, dried and alcohol extracts.
Cytotoxicity
22. The cytotoxicity of ginger has been investigated with varied results. Plengsuriyakarn et al. (2012) examined cytotoxicity in Cholangiocarcinoma (CCA) cell line 6 (CL-6), hepatocarcinoma (HepG2) and normal human renal epithelium (HRE) models using calcein-AM release and Hoechst 33342 assays. The median inhibitory concentration, (IC50) and value for cytotoxicity of the crude ethanolic extract of ginger were 10.95 and 53.15, μg/ml respectively.
23. Zaeoung et al. (2005) reported that the IC50 of ginger was higher than 39.2 µg/ml against breast (MCF7) and colon (LS174T) cell lines. Abudayyak et al. (2015) found the aqueous and methanol extracts of ginger exhibited no cytotoxic activity when assessed using an MTT test (a colourimetric assay for assessing cell metabolic assay) in the rat kidney, NRK-52E cell line. The chloroform extract resulted in an IC50 value of 9.08 mg/mL.
24. However, it was noted that the inhibitory concentration (IC50) values presented in the studies reviewed were based on a small amount of data, from only six different cell lines and therefore firm conclusions could not be drawn. Also, the purpose of most of these studies was an attempt to identify possible anti- cancer agents, rather than as an assessment on the safety of ginger as a supplement and therefore relevant endpoints would not have been assessed.
Mutagenicity
25. Nakamura and Yamamoto (1982) found that the juice of ginger rhizome possessed both mutagenic and anti-mutagenic properties, and that 6-gingerol in particular was a powerful mutagen. The group also demonstrated that 6-shogaol was much less mutagenic (strain Hs30 of Escherichia coli) than 6-gingerol (Nakamura & Yamamoto 1983). In a Salmonella typhimurium reverse mutation (Ames) assay, the urine of rats fed diets containing 0.5, 1 and 5% powdered ginger for 1 month and exposed to benzo(a)pyrene was found to display a significant reduction in the mutagenicity as indicated by a reduced number of TA98 and TA100 revertants at all ginger concentrations (Nirmala et al. 2007) when tested in an Ames assay.
26. In another Ames assay, an ethanol extract of ginger (Soudamini et al. 1995) and an essential oil from ginger (Sivaswami et al. 1991) demonstrated mutagenic activity in S. typhimurium strains TA 100 and TA 1535 at concentrations of 25-50 mg/plate and 5-10 mg/plate, respectively. Similarly, an ethanolic ginger extract at concentrations between 10 and 200 μg/plate, and gingerol and shogaol were mutagenic in strains TA 100 and TA 1838 with metabolic activation by rat liver S9 fraction, while zingerone did not display mutagenic effects (Nagabhushan et al. 1987).
27. Abudayyak et al. (2015) found the aqueous ginger extract exhibited mutagenic activity when assessed using the Ames assay on S. typhimurium TA98 (-S9) strains. No activity was observed with the chloroform and methanol extracts.
28. Based on the available data, ginger showed some mutagenicity in TA 100, TA 1535, and TA 98 strains, but this is low compared with established mutagens. Ginger is not shown to be mutagenic in vivo (Nirmala, Prasanna Krishna and Polasa, 2007).
Acute toxicity
29. An acute toxicity study carried out by Malik and Sharma on male Wistar rats showed no signs of toxicity or mortality (2011). The animals were administered doses of 250, 500 and 1000 mg/kg lyophilised ginger powder by gastric gavage. The authors stated that the three dose levels used in the study corresponded to 5, 10 and 20% of the NOAEL of the powder (5000 mg/kg).
30. Plengsuriyakarn et al. also examined acute and subacute toxicity in hamsters. Sixty hamsters (nine groups of 5 male and 5 female) were fed either 1000, 3000 or 5000 mg/kg bw ethanolic ginger extract, resuspended in a distilled water-Tween-80, mixture 4:1, v:v, by oral gavage and observed for 14 days (acute toxicity) or 30 days (subacute toxicity). The group concluded that there was an absence of any toxicity at maximum dose of 5 g/kg bw during the investigation period.
Short term repeat dose studies
31. Rong et al. (2009) evaluated the safety of powdered Japanese ginger (mainly containing 6-gingerol galanolactone and 6-shogaol) by conducting a 35-day toxicity study in rats. Both male and female rats were treated with 500, 1000 and 2000 mg/kg bw/day by gavage. The results demonstrated that oral administration of up to 2000 mg/kg to male and female rats did not result in any increase in mortality, or changes to behaviour, growth, the general condition of the animals (including: changes in skin, fur, eyes, and mucous membranes, occurrence of secretions, excretions and autonomic activity), food and water consumption. It was only at the highest dose tested (2000 mg/kg), that ginger led to slightly reduced absolute and relative weights of testes (by 14.4% and 11.5%, respectively). No effects were apparent in the females.
32. The effect of oral and intraperitoneal administration of aqueous extracts of ginger root over 28 days in female rats at two dose levels (50 mg/kg and 500 mg/kg) was examined for haematological, serum and systemic toxicity (Alnaqeeb et al. 2003). Neither oral nor intraperitoneal administration resulted in mortality. Orally administered aqueous ginger extract resulted in increased levels of serum aspartate aminotransferase (AST) and decreased levels of alanine aminotransferase (ALT).
33. Jeena et al., conducted a sub chronic toxicity study of the essential oil of ginger in Wistar rats following oral administration at concentrations of 100, 250, and 500 mg/kg per day once daily for 13 consecutive weeks to assess the oral safety of ginger oil (2011). No mortality was observed. No unusual changes in behaviour or locomotor activity were observed during the period of the study, nor were any abnormal changes observed in the relative organ weights of liver, kidney, spleen, lungs, brain, and stomach with respect to body weight in ginger oil-treated animals when compared to vehicle control animals.
34. An increase in serum sodium levels was observed in male rats treated with 500 mg/kg per day but in the absence of changes in sodium levels in females, this change was not considered significant. A slight increase in total bilirubin was observed in female rats treated with ginger oil along with a decrease in AST and ALT levels however, there was no significant changes in hepatic function parameters such as alkaline phosphatase, total protein, albumin, and globulin content.
Reproductive and developmental toxicity
In vitro studies
35. Mohammed et al investigated the effects of herbal extracts, including ginger and 6-gingerol, on chick embryonic heart micromass and mouse D3 embryonic stem cell systems (ESD3) (2016). The team observed that the use of ginger herbal remedies in the first trimester of pregnancy may affect foetal development. However, 6-gingerol-treated primary embryonic chick cardiomyocytes showed no significant changes in contractile and cellular activity or changes in total protein content in comparison to the control.
36. At concentrations of 0.75–6 µM, 6-gingerol treated primary embryonic chick cardiomyocytes exhibited no significant changes in contractile activity, cellular activity or changes in total protein content in comparison to the control. At concentrations of 12.5–50 µM, inhibition in contractile activity was observed at 48h. All high 6-gingerol concentrations, 12.5–100 µM, tested in micromass, significantly altered both the cellular activity and protein content in a dose-dependent manner.
37. The same concentrations of 6-gingerol were used to treat the ESD3, which showed a significant decrease in cardiomyocyte differentiation for all tested concentrations except 0.75 µM. The cellular activity and protein content of stem cell-derived cardiomyocytes also exhibited a significant decrease with increased 6-gingerol concentration exposure. The 6 µM dose showed almost no differentiation in the morphological score on days 10 and 11, which was considered an anomaly. However, a small amount of differentiation was observed on day 12.
Animal studies
38. To date, the number of studies on the safety of the use of ginger supplements during pregnancy is limited. The ginger component 6-gingerol, was highlighted to affect some essential embryonic developmental processes, such as the disruption of angiogenesis. Kim et al, demonstrated the ability of 6-gingerol to inhibit proliferation and tube formation of primary cultured human endothelial cells in rat aorta by down regulation of cyclidin D and the ability to inhibit tumour growth in mice through its anti-angiogenic activity (2005).
39. The animal studies on reproductive toxicity considered in TOX/2021/26 reported a number of findings, including reduced maternal weight gain, increased fetus weight, increased serum testosterone level in F1 generation males and an increase in embryonic loss.
40. The teratogenicity of EV.EXT 33, a patented Zingiber officinale extract (comprising 6-gingerol, 8-gingerol, 10-gingerol, 6-shogaol, and 8-shogaol, which made up 1.9 w/w of the extract) was investigated in Wistar rats, (Weidner & Sigwart, 2001). The extracts were administered orally by gastric intubation at concentrations of 100, 333 and 1000 mg/kg, to three groups of pregnant rats from days 6 to 15 of gestation. Their bodyweight, food and water monitored during the treatment period. The study concluded that treatment with EV.EXT 33 during the period of organogenesis resulted in neither maternal nor developmental toxicity at daily doses of up to 1000 mg/kg bw.
41. Shalaby and Hamowieh investigated fertility, serum testosterone and acute toxicity of ginger in rats (2010). One hundred and twenty male Sprague Dawley rats, separated into groups of 10, were orally administered either water (prepared using 100 g dry ginger roots soaked in 500 ml water or 500 ml methyl alcohol 90%) or methanolic extracts in graded doses ranging from 5 to 17.5 g/kg bw (gavage doses were not specified). Following dosing, the number of dead mice in each group after 48 hours of observation were recorded. The oral Lethal Doses (LD50) of the methanolic and water extracts were calculated to be 10.25 and 11.75 g/kg bw respectively. No symptoms of toxicity were observed at does up to 5 g/kg bw. Both extracts increased fertility index, sexual organ weight, and sperm motility and count after 65 consecutive days (see below).
42. To investigate the effect of ginger extracts on serum testosterone levels, male rats had their fertility reduced by inducing diabetes, a condition shown to reduce male fertility. The aim was to see whether ginger, with its antioxidant and androgenic effects, would restore fertility. Rats were rendered diabetic by subcutaneous injection of 120 mg/kg bw alloxan for 3 days, were administered methanolic extracts of ginger for 65 days at doses of 100 and 200 mg/kg bw/d. Testosterone levels increased to 4.08 ± 0.10 and 7.13 ± 0.14 ng/dL (both significant at P < 0.001) compared to the diabetic control group who had levels of 3.30 ± 0.03 ng/dL. Serum testosterone levels also increased in rats given water extracts (150 and 300 mg/kg bw) were determined to be 4.06 ± 0.03 and 5.04 ± 0.08 ng/dL (both significant at P < 0.001 when compared to the diabetic control group) respectively.
43. The team also investigated fertility with regards to fertility index (for each male this was calculated as percentage of number of females that become pregnant in relation to number of mated females) and spermatogenesis. Rats were orally administered methanolic extracts at doses of 100 and 200 mg/kg bw for 65 consecutive days and water extracts at doses of 150 and 300 mg/kg bw and compared to a diabetic control group.
44. Histopathological examination of the testes of diabetic rats showed mild to moderate degenerative changes of spermatogenic cells, diffuse oedema and incomplete arrest of spermatogenesis. The testes of rats orally administered 300 mg/kg bw of water extract of ginger roots showed mild degeneration of spermatogenic cells and slight oedema of interstitial cells. The testes of rats receiving orally 200 mg/kg bw of methanolic extract of ginger roots showed nearly normal seminiferous tubules, showing fewer signs of degradation, suggesting a LOAEL of 200 mg/kg bw/day for the methanolic extract. The team concluded that the results suggest the intake of ginger root as a drink may be useful for diabetic patients suffering from sexual impotency.
45. The above study has been included for completeness and as any general mechanisms may be more widely relevant: This is consistent with the findings of Hosseini et al (2015) – see paragraph 29, Annex B.
46. No additional reproductive studies were identified. Therefore, any point of departure for ginger would need to be based on the animal studies discussed in TOX/2021/26 and reproduced in paragraphs below.
47. Reproductive and developmental toxicity has also been investigated in rat studies. In a study by Wilkinson (2000), three groups of pregnant Sprague-Dawley rats were administered either a control (unspecified), or 20 g/L or 50 g/L ginger tea - prepared by the infusion of grated ginger in water via their drinking water - during days 6 to 15. No further details were provided regarding specific compounds of interest. While no maternal toxicity was observed, embryonic loss in the treated groups was found to be double that of the controls. Exposed foetuses were found to be significantly heavier than controls and showed no gross structural malformations. The results of this study suggest that in utero exposure to ginger tea results in early embryonic loss and increased growth in surviving foetuses.
48. Hosseini et al. investigated the effect of ethanolic ginger extract on serum testosterone, LH and FSH as well effect on spermatogenic cell lines in male mature offspring rats (2015, abstract only). In this study, 72 female rats, sorted into 9 groups were orally administered of alcoholic extract of ginger at doses of 50, 100 and 200 mg/kg bw, during their neonatal and perinatal periods versus saline as a control. Following puberty, LH, FSH, cell numbers of Sertoli, spermatogonia, spermatocyte and spermatids were counted in 8 male rat offspring from each group. Ginger was found to significantly increase testosterone levels and the number of spermatogenic cells and at doses of 100 and 200 mg/kg bw, alcoholic extract of Ginger significantly reduced the FSH and LH compared to control groups. The authors concluded that “the oral consumption of Ginger during pregnancy and lactation dose-dependently increase the level of testosterone and the number of spermatogenic cells.”
49. The teratogenicity of EV.EXT 33, a patented Zingiber officinale extract (comprising 6-gingerol, 8-gingerol, 10-gingerol, 6-shogaol, and 8-shogaol, which made up 1.9 w/w of the extract) was investigated in Wistar rats, (Weidner & Sigwart, 2001). The extracts were administered orally by gastric intubation at concentrations of 100, 333 and 1000 mg/kg, to three groups of pregnant rats from days 6 to 15 of gestation. Their bodyweight, food and water monitored during the treatment period. The study concluded that treatment with EV.EXT 33 during the period of organogenesis resulted in neither maternal nor developmental toxicity at daily doses of up to 1000 mg/kg bw.
50. Dissabandara & Chandrasekara (2007) also examined the effect of powdered ginger extract administered prenatally on the postnatal development of rats. A period of administration of the dry powdered extract orally at doses of 500 mg/kg/day or 1000 mg/kg/day (control not specified) during days 5 to 15 of gestation resulted in a lower intake of food and water and lower weight gain in the ginger treated group, suggesting that maternal administration of ginger during mid pregnancy resulted in reduced maternal weight gain and increased embryonic loss without affecting the postnatal growth and physical maturation of the surviving offspring.
51. ElMazoudy and Attia (2018) investigated the effect of powdered dried ginger root on the oestrus cycle and implantation in female mice. ICR mice, orally dosed at 250, 500, 1000, or 2000 mg/kg bw/d aqueous ginger extract. These were investigated in four different experiments: the main study of outcomes (treatment for 90 days and throughout mating and gestation), a 35-day treatment study evaluating effects on the oestrous cycle. The third and fourth intended antifertility and abortifacient loss (20 days treatment). In the main study, the dams were sacrificed on gestation day 20. One mortality was recorded in the 100mg/kg bw/d group on gestation day 18 and two mortalities in the 2000 mg/kg bw/d group at day 16. There was also a significant reduction in body weight change in these two dose groups compared to the control group; however, food consumption was comparable.
52. In the study investigating the oestrus cycle, a significant reduction in the numbers of oestrus cycles was observed at the highest dose group, with the length of the oestrus cycle in this group being significantly prolonged (10.05 ±0.8) days compared with (4.99 ± 0.5) days recurrent and successive oestrous cycles in control mice. At the highest dose level, the length of the oestrous cycle was prolonged with a significant decrease in the duration of diestrous-metestrus (luteal) phase and prolonged proestrus-estrus (ovulatory) phase. In the study investigating pre-implantation loss, a significant decrease in the number of corpora lutea was observed at the highest dose group. Implantation failure was also increased by 36% compared to the control group and pre-implantation loss at this dose group was also 16.59% higher than the control group. The authors considered that this may reflect a dose-depend antifertility (anti-implantation) effect.
53. Regarding fertility and developmental outcomes, the female copulation index was significantly reduced at 2000 and 1000 mg/kg bw/d groups, whereas the female pregnancy index was significantly decreased only at the highest dose. The number of implantation sites and live fetuses in the 2000 mg/kg bw/d group was lower than the other treated and control groups. An increase in fetal resorption and post implantation loss was also seen at the highest dose group. There was no evidence of fetal malformations however growth retardation, reduced pup weight and delay in the crown-rump length was observed at this dose group as well. Finally, changes in ovarian histopathology were observed at 2000 mg/kg bw/d, following 90 days of treatment. Ovarian follicle atresia was observed. The atretic follicles contained cell debris and there was haemorrhage in the antral cavity.
54. Additionally, degenerated primordial follicles with pyknotic nuclei forming polycystic ovaries were noted. Deteriorated follicles were observed as a detaching of layers of granulosa cells from the basal membrane by dilation of zona pellucida and with evidence of apoptosis in damaged ova follicular nuclei were non-visible. The authors considered the above observations as evidence that ginger possesses anti-ovulation properties. Overall, the authors concluded that ginger impairs the normal growth of corpus luteum because of progesterone insufficiency during early pregnancy and that the results suggested that ginger can disrupt the oestrous cycle and blastocyst implantation without teratogenesis. They considered the highest NOAEL to be 500 mg/kg bw.
55. The Committee considered the animal studies to be inconclusive. Plengsuriyakarn et al., examined acute and subacute toxicity in hamsters (2012). Sixty hamsters (nine groups of 5 male and 5 female) were fed either 1000, 3000 or 5000 mg/kg bw ethanolic ginger extract, resuspended in a distilled water-Tween-80, mixture 4:1, v:v, by oral gavage and observed for 14 days (acute toxicity) or 30 days (subacute toxicity). The group concluded an absence of any toxicity at maximum dose of 5 g/kg bw during the investigation period.
56. ElMazoudy and Attia (2018) noted reductions in bodyweight and mortalities in mice dosed up to 2000 mg/kg bw/day and Alnaqeeb et al., (2003), observed increases in serum aspartate aminotransferase (AST) in female rats dosed up to 500 mg/kg. However, the Committee noted that the database was limited and on the basis of the available information, more data would be needed in order to allow for a robust investigation of the effects described above. Therefore, at present, the Committee were unable to determine a point of departure, to reach a conclusion.
Human studies
57. The COT considered a number of epidemiological studies investigating the use of ginger during pregnancy (TOX/2021/26). For the most part, few studies explicitly addressed the safety of ginger consumption during pregnancy. Most were focused on the use of ginger as a treatment for nausea (Fischer-Rasmussen et al., 1990; Smith et al., 2004; Ensiyeh et al., 2009), age-related neurological disorders or pregnancy-induced sickness and therefore focused on efficacy (Willetts et al., 2003; Stanisiere et al., 2018). However, safety was considered in a few studies. The studies considered by the Committee included observational and randomised clinical studies, lasting from 4 days to 20 weeks in duration (Vutyavanich et al., 2001; Portnoi et al., 2003). Ginger in various forms was investigated in doses ranging from 750 mg/day to the equivalent of 7 g/day.
58. The study results in pregnant women were also varied and the overall findings inconclusive. Findings reported included abdominal discomfort, vomiting and diarrhoea. There were reports of incidences of spontaneous abortion (Portnoi et al., 2003, Ensiyeh et al., 2009), however, this effect was observed in both the treated and control groups and therefore, cannot directly be attributed to the consumption of ginger. Portnoi et al., reported 8 spontaneous abortions in the comparator group, compared to 3 occurring in the group taking ginger and Ensiyeh et al., reported 2 spontaneous abortions in the ginger group compared to 1 in the group taking vitamin B6. This study reported no effects of defects post-partum following exposure to ginger.
Human studies - exposures in pregnancy
59. In their 2003 review of interventions for nausea and vomiting in early pregnancy, Jewell and Young concluded that maternal consumption of ginger shows no evidence of teratogenicity in infants (Jewell and Young, 2003). More recently, Stanisiere et al. (2018) conducted a review of the safety and efficacy of ginger rhizome for decreasing nausea and vomiting in women during early pregnancy. This review was based on systematic literature searches until the end of December 2017. Most of the studies included in this review have already been included in this draft statement. Some recent studies have been conducted evaluating the effectiveness and safety of ginger in pregnancy, and these will be discussed in detail. Overall, most studies reported gastrointestinal effects such as abdominal discomfort, vomiting and diarrhoea. Other effects included dizziness, headaches and drowsiness with some more serious effects such as spontaneous abortion also being reported in 5 out of the 14 randomized clinical studies. The review by Jewell and Young focuses on the reported effects rather than statistical significance, therefore more details on the studies reporting more serious effects are given below.
60. In a double-blind randomised crossover trial, 27 women were administered capsules containing either 250 mg ginger in powdered root form or 250 mg lactose as a placebo, four times per day, for four days followed by a wash out period of 2 days prior to a further 4 days administration of ginger or placebo (Fischer-Rasmussen et al., 1990). Two subjects did not carry to term: One subject from the ginger group had a spontaneous abortion, one elected. Of the remaining 25 subjects, no adverse effects were observed.
61. Of the available human studies, few explicitly addressed the safety of ginger consumption during pregnancy, most being incidental to other studies. In a double-blind study by Vutyavanich et al. (2001), 32 women were given 1 g of dried ginger in capsule form for 4 days. Of those in the ginger group, one spontaneous abortion was reported compared to 3 in the placebo group. Equally, for delivery by caesarean section, there was no difference between both groups. No congenital abnormalities were observed in all babies carried to term. The group concluded that there were no significant adverse effects of ginger on pregnancy outcome.
62. An observational study in humans examined 187 pregnant women who took ginger in their first trimester and compared them to 187 pregnant women exposed to nonteratogenic drugs that were not antiemetic drugs. The results suggested that the ginger group did not have an increased rate of major malformations above the baseline rate of 1%–3% (Portnoi et al., 2003). Three major malformations were reported in the ginger group, ventricular septal defect (VSD), right lung abnormality, and kidney abnormality (pelviectasis) and one child was diagnosed with idiopathic central precocious puberty at age 2 years. The mother was reported to have taken 250 mg of ginger in capsules four times a day from 11 to 20 weeks of gestation in addition to dimenhydrinate and doxylamine/vitamin B6 (Diclectin) during the first trimester of pregnancy. No significant difference between the two groups in terms of live births, spontaneous abortions, stillbirths, therapeutic abortions, birth weight, or gestational age were reported, however the comparison group had more infants weighing less than 2500 g and the ginger group had 8 sets of twins.
63. Willetts et al. examined the effect of ginger on pregnancy induced nausea (2003). 120 women less than 20 weeks pregnant, were given 125 mg ginger extract (EV.EXT35; equivalent to 1.5 g of dried ginger) or a placebo four times per day for 4 days. Three spontaneous abortions were observed in the group receiving ginger compared to those in the placebo group. Whilst also examining the use of ginger in the treatment of nausea and vomiting in pregnancy, Smith et al. noted 3 spontaneous abortions in the group taking 1.05 g ginger compared to 9 in the group taking 75 mg B6 daily for 3 weeks (2004).
64. Ensiyeh et al, investigated the effectiveness of ginger versus B6 for treatment of NVP (2009) in women before 17 weeks’ gestation. 70 women were randomised to receive either ginger at a dose of 1 g per day or B6 and 40 mg per day for 4 days. The ginger group reported 2 spontaneous abortions, compared to one in the B6 group. Of the babies brought to term, no congenital anomalies were observed, and all babies were discharged in good condition.
65. The COT considered the mode of action of the purported benefits of ginger on nausea. It was theorised that ginger might decrease prostaglandin levels, which were linked to nausea.
66. The Committee noted the potential effect of ginger on the prostaglandin pathway, in particular Cyclooxygenase-1 (COX1) and Cyclooxygenase-2 (COX2) inhibition and how this may affect early pregnancy. One study examining the effects of ginger extracts on prostaglandin E2 (PGE2) production in vitro (Lantz et al. 2007) demonstrated that crude organic extracts (dichloromethane-methanol, 1:1 v/v) of ginger were capable of inhibiting PGE2 production and that the compounds may act at several sites. The most potent effect on lipopolysaccharide (LPS) induced prostaglandin production was noted at less than 0.1 µg/ml. It was noted that the half maximal inhibitory concentration (IC50) values for a range of components were given, and it was demonstrated that the components mainly acted on COX-2. The COT concluded further studies would be needed to determine the role of increased prostaglandin levels in the early termination of pregnancy.
67. Overall, it was concluded that there were limited data. The human data presented were not strongly indicative of any toxicological concern but there were some indications of possible effects and many uncertainties. Ginger did not appear to be systemically toxic but reprotoxic effects have been reported in animal studies. However, there is no significant evidence for this outcome in human studies.
Lactation
68. With respect to lactation, the focus of available studies (Lamxay et al., 2011; Kaygusuz et al., 2021; Dilokthornsakul et al., 2021) has been on the effect of ginger on milk production and volume rather than safety and therefore, the effect of exposure during lactation has not been fully investigated.
Effect on Cytochrome P450 (CYP) Enzymes and Herb-Drug Interactions
69. CYPs are a family of enzymes responsible for the biotransformation of several drugs. Induction or inhibition of CYP enzymes is a major determinant of the occurrence of drug-drug interactions.
In silico
70. Qiu et al. (2015) investigated the molecular interactions between 12 main active components (6-gingerol, 8-gingerol, 10-gingerol, 6-shogaol, 8-shogaol, 10-shogaol, ar-curcumene, β-bisabolene, β-sesquiphelandrene, 6-gingerdione, (-)-zingiberene, and methyl-6-isogingerol) and human cytochrome P450 (CYP) 1A2, 2C9, 2C19, 2D6, and 3A4 and attempted to predict the absorption, distribution, metabolism, excretion, and toxicity (ADMET) of the 12 ginger components using computational methods and literature searches. This study suggests that ginger components may regulate the activity and expression of various human CYPs, resulting in alterations in drug clearance and response.
71. These results could potentially be significant in pregnant women on medication, who are using ginger as a remedy for nausea in the early stages of pregnancy.
In vitro studies
72. Ginger extracts and the major components thereof - 6-gingerol (6G), 8-gingerol (8G), 10-gingerol (10G) and 6-shogaol (6S) - were investigated in in vitro models and shown to have an inhibitory effect on CYP isoenzymes CYP3A4, CYP2C9 (Kimura et al., 2010) CYP2C19 (Kim et al., 2012) and CYP1A2 and CYP2C8 with IC50 values as low 1µM, (e.g., 6-shogaol on CYP1A2; Mukkavilli et al., 2014).
Animal studies
73. Several reports have been published on the pharmacological properties of ginger, with varying results. Studies have examined herb-drug interaction in animal models, (Okonta et al., 2008; Egashira et al., 2012) although some studies have questionable results.
74. A study into the effect of ginger on the pharmacokinetics of metronidazole was studied by Okonta et al., using rabbits (2008). In a two-phase study, five healthy local strain rabbits (3 females, two males) were each given 3 mg/kg oral metronidazole. Following a 2-week washout period, the rabbits were given 1 ml/kg of ginger extract orally daily for 3 days and immediately given 3 mg/kg metronidazole per oral on the third day. Ginger significantly increased the absorption and plasma half-life, and significantly decreased the elimination rate constant and clearance of metronidazole.
75. Egashira et al., reported the interaction between ginger juice and tacrolimus in rats (2012). Tacrolimus (0.6 mg/kg) was administered intraduodenally in male Sprague-Dawley rats 1 hr following oral administration of 10 mL/kg 50% ginger juice or water. Pre-treatment with ginger juice was found to significantly increase tacrolimus blood concentrations compared to those pre-treated with water or orange juice.
76. The possible herb-drug interaction of ginger crude extract on glibenclamide and insulin was investigated by Al Omari et al., along with its hypoglycaemic and antihyperglycemic effects in normoglycemic- and streptozotocin-induced (STZ) diabetic rats (2012). Ginger crude extract was administered to normoglycemic male rats as a single dose (1 day) and as a daily dose for 1 week. STZ diabetic rats were treated with the same GCE concentrations (25, 50 and 100 mg/kg bw) together with glibenclamide (5 mg/kg bw) or insulin (1.2 IU/kg bw).
77. Single administration of ginger crude extract showed a significant decrease in blood glucose level (BGL) in normoglycemic rats after 1 and 2 hours (50 mg/kg bw). In STZ- diabetic rats ginger crude extract (25 and 50 mg/kg bw) decreased non-fasting BGL (N-FBGL) significantly at 1.5, 2.5, 3.5 and 4.5 hours. Glibenclamide (5 mg/kg bw) in combination with ginger crude extract at doses 25 or 50 mg/kg bw exhibited a significantly reduction in the N-FBGL 26.3% and 25.1% respectively after 4.5 hours, compared to glibenclamide alone which exhibited a 7.9% reduction.
Human studies
78. Human data showed possible interactions with medicines, including antibiotics, immunosuppressants, and anticoagulant medications. Although, in some cases, multiple concomitant medications were being used therefore, the effects observed cannot necessarily be directly attributed to ginger supplementation (Rubin et al., 2019).
79. Conversely, whilst investigating the effects of ginger on the pharmacokinetics or pharmacodynamics of warfarin and the effect of ginger on clotting status, Jiang et al., (2005), found that neither the pharmacokinetics nor pharmacodynamics of warfarin were affected in healthy males who were treated with a single 25 mg dose of warfarin, following 7 days of pretreatment with ginger tablets (3 tablets, 3 times per day, each capsule containing extract equivalent to 0.4 g of ginger rhizome powder). Furthermore, ginger had no effect on international normalized ratio (INR) or ex vivo platelet aggregation in response to arachidonic acid.
80. Ginger was found to have a significant inhibitory effect on CYP3A4, CYP2C9, and P‐glycoprotein activities in vitro (Kimura et al., 2010; Zhang and Lim, 2008). It was this effect that was thought to be responsible for reported hepatic cytolysis in a 48-year-old woman being treated with crizotinib. The patient, who was being treated with 250 mg crizotinib twice a day, had been taking ginger as a tea (amounts unknown) concomitantly during treatment. A subsequent diagnostic evaluation showed an increased crizotinib concentration, 1.8-fold higher than that measured two months prior.
Anti-platelet aggregation activity
81. Several reports have been published on the pharmacological properties of ginger, with varying results. The potential effect of ginger extract and components thereof on the reduction of platelet aggregation and their potential antithrombotic activity has been noted as a concern in both literature and by health professionals.
82. Ginger was reported to have antiplatelet activity (Srivastava, 1986,1989; Young et al., 2006), with some studies reporting effects in animals at doses of 500 mg/kg bw (Thomson et al., 2002). Ginger was found to inhibit platelet thromboxane and prostaglandin endoperocides (PGF2α, PGE2 and PGD2) in human platelets, in a dose-dependent manner (Srivas, 1984).
83. With regards to the relevance of such effects in pregnancy, literature reports note that pregnancy is associated with an increased incidence of thrombotic events; mainly related to a pro-thrombotic state, physiologically useful to reduce bleeding at delivery. These changes are more pronounced in the third trimester (Patti et al., 2014). It has also been hypothesised that antiplatelet agents might prevent or delay the development of pre-eclampsia (Duley et al., 2019). The implications and clinical significance of the anti-platelet activity of ginger exposure during different stages of pregnancy remain undetermined.
84. This further highlighted the need to differentiate exposure from the normal diet to that from supplements. Members noted that associations with haemorrhagic effects were reported following supplemental exposure to ginger, (Kruth et al., 2003; Rubin et al., 2019; Al Askar et al., 2020) though these were inconclusive.
85. A study by ElMazoudy and Attia (2018) linked follicular failure to haemorrhagic effects in a study investigating the effect of dried ginger root on the oestrus cycle and implantation, in female mice. The authors concluded that ginger impairs the normal growth of the corpus luteum because of progesterone insufficiency during early pregnancy and that the results suggested that ginger can disrupt the oestrous cycle and blastocyst implantation without teratogenesis. They considered the highest NOAEL to be 500 mg/kg bw. The COT noted that this might be worth further investigation. However, it was also noted that other factors could be contributing to the results observed and the study results were inconclusive.
In vitro studies
86. Srivastava reported an effect of ginger extracts on in vitro platelet aggregation (1986). Ginger extracts in water, n-hexane, chloroform, and ethyl acetate were shown to inhibit platelet aggregation using arachidonic acid (AA), epinephrine, adenosine diphosphate (ADP), and collagen as agonists.
Animal studies
87. The effect of an aqueous ginger extract on platelet thromboxane-B2 (TBX2) and prostaglandin-E2 (PGE2) production was studied by Thomson et al. (2002). Adult female Sprague-Dawley rats were administered an aqueous extract of raw ginger at either 50 mg/kg or 500 mg/kg daily, by either oral gavage or intraperitoneally (IP) for a period of 4 weeks. A dose of 50 mg/kg ginger administered orally, or IP did not result in any significant reduction in serum thromboxane-B2 levels when compared to saline-treated control groups but doses at 500 mg/kg significantly reduced TBX2 levels in serum.
88. A non-significant reduction in the level of TXB2 was observed when ginger was injected IP. However, levels were not significantly different from the TXB2 levels in control rats that had received saline. 50 mg/kg of ginger administered orally resulted in serum PGE2 levels being significantly reduced however, 500 mg/kg was found to be more effective in reducing PGE2 synthesis. PGE2 levels were reported to be significantly lower than the saline control in rats given 500 mg/kg ginger extract both orally and IP.
89. The composition of ginger extracts also appears to vary according to whether ginger is fresh or dried. Suekawa et al., demonstrated that (6)-shogaol, a principal component mainly found in dried ginger, inhibited carrageenan-induced swelling of rat hind paw, AA-induced platelet aggregation in rabbit and prostaglandin PGI2 release in rat aorta, suggesting a potential inhibitory action on cyclooxygenases (COX) in both platelets and aorta tissue (1986, abstract only).
Human studies
90. Srivastava (1989) investigated the effect of fresh ginger on blood platelet thromboxane synthesis in humans. In a study on 7 women aged between 25-65 years, where volunteers consumed ~5g of fresh ginger for 7 days. Ginger was found to inhibit eicosanoid biosynthesis in vivo.
91. Krüth et al. reported the possible over-anticoagulation resulting from a possible ginger-phenprocoumoun interaction (2003). A 76-year-old woman on long-term phenprocoumon therapy presented with epistaxis and an international normalized ratio (INR) of >10. Partial thromboplastin time (PTT) was also found to be prolonged (84.4 seconds; normal <35). For several weeks prior to the event, the woman had a regular ginger intake of dried ginger prices and tea from ginger powder. Following treatment with vitamin K, the patient’s INR and PTT returned to within therapeutic range.
92. Young et al. investigated the synergistic effect of ginger and nifedipine on anti-platelet aggregation in healthy volunteers aged 25-60 years old and hypertensive individuals aged 35-60 years old (2006). In a five-part study, the two groups comprising of 10 males and 10 females were administered 75 mg of acetylsalicylic acid (ASA), 1 g of ginger, 10 mg nifedipine, 1 g ginger and 10 mg nifedipine in combination and 1 g ginger and 75 mg ASA in combination daily for one week each following a washout period (7 days following ASA administration, 10 days thereafter).
93. Platelet aggregation in the presence of collagen ADP and epinephrine was 44.1%, 44.5% and 42.1% in normal subjects and 64.2%, 67.7% and 62.9% in hypertensive patients, respectively. Platelet aggregation induced by collagen, ADP or epinephrine was found to be higher in hypertensive patients than normal patients. Following administration of ginger alone, platelet aggregation was measured as 35.2%, 37.8%, 35.9% with collagen, ADP and epinephrine respectively. When administered ginger and nifedipine in combination, the percentage inhibition of platelet aggregation induced by collagen, ADP and epinephrine were 79.8%, 75.2%, 69.3% respectively.
94. Rubin et al. (2019) reported the possible effect of ginger supplementation on the (INR) in a woman taking warfarin. The 70-year-old female, who had been taking clonazepam 1 mg, metoprolol succinate 25 mg, paroxetine 10 mg, phenytoin 30 mg, rosuvastatin 20 mg, warfarin 7.5 mg daily, and warfarin 10 mg once day per week, presented with an INR of 8, an increase from 2.7 one month prior after taking a 48 mg ginger supplement daily. A week following cessation of the ginger supplement, the INR declined to 2.6.
95. Al Askar et al. (2020) investigated the effect of ginger on platelet aggregation using agonists adenosine diphosphonate, arachidonic acid, collagen, ristocetin and epinephrine. Forty healthy male and female participants were randomized (1:1) to consume ginger tea at an amount of 4 g in 150 ml of boiling water once daily vs. 4 g twice daily for five consecutive days. 4 g of ginger powder administered daily resulted in reduced platelet aggregation in subjects using epinephrine only. Platelet aggregation inhibition was also found to be higher in women using arachidonic acid.
96. Ginger, in powder form (5 g per day), was demonstrated to significantly (P<0.001) decrease ADP- and epinephrine-induced platelet aggregation in healthy male subjects who were fed 100 g of butter daily for seven days (Verma et al., 1993). Conversely, Bordia et al., found that 4 g powdered ginger administered daily over the course of 1.5 and 3 months had no effect on ADP and epinephrine-induced platelet aggregation in individuals with coronary artery disease (CAD). However, a single 10g dose of powdered ginger, administered to CAD patients resulted a significant decrease in induced platelet aggregation (1997).
97. Conversely, Lumb found that a dose of 2g of ginger in powder form daily produced no significant differences in platelet aggregation/function than the placebo and concluded that these effects may be dose dependant or attributed to fresh ginger (1994). Whilst investigating the effects of ginger on the pharmacokinetics or pharmacodynamics of warfarin and the effect of ginger on clotting status in adult males, Jiang et al., also found that the pharmacokinetics nor pharmacodynamics of warfarin were not affected in healthy males who were treated with a single 25 mg dose of warfarin, following 7 days of pretreatment with ginger tablets (3 tablets, 3 times per day, each capsule containing extract equivalent to 0.4 g of ginger rhizome powder) (2005). Furthermore, ginger had no effect on international normalized ratio (INR) or ex vivo platelet aggregation in response to arachidonic acid.
Effects on blood pressure
In vivo
98. Ghayur and Gilani (2005) reported that a crude extract of ginger induced a dose-dependent (0.3–3 mg/kg) fall in arterial blood pressure of anesthetized Sprague-Dawley rats (2005). In Guinea pig paired atria, the crude extract exhibited cardio-depressant activity on the rate and force of spontaneous contractions. In rabbit thoracic aorta preparation, the crude extract relaxed the phenylephrine induced vascular contraction at a dose 10 times higher than that required against K+-induced contraction (80 mM).
99. Ca2+ channel-blocking (CCB) activity was confirmed when the crude extract shifted the Ca2+ dose–response curves to the right similar to the effect of verapamil. It also inhibited the phenylephrine (1 mM) control peaks in normal-Ca2+ and Ca2+-free solution, indicating that it acts at both the membrane-bound and the intracellular Ca2+ channels. When tested in endothelium-intact rat aorta, it again relaxed the K+-induced contraction at a dose 14 times less than that required for relaxing the PE-induced contraction. The vasodilator effect of the crude extract was endothelium-independent because it was not blocked by Nω-nitro-L-arginine methyl ester hydrochloride (L-NAME) (0.1 mM) or atropine (1 mM) and also was reproduced in the endothelium-denuded preparations at the same dose range. These data indicate that the blood pressure-lowering effect of ginger is mediated through blockade of voltage-dependent calcium channels.
Effect on Prostaglandins
In vitro
100. Ginger extracts, along with many gingerols and shogaols have been shown to suppress prostaglandin synthesis in vitro, through inhibition of cyclooxygenase (Jolad et al. 2005; Pan et al. 2008; Dugasani et al. 2010).
101. Lantz et al. investigated the anti-inflammatory effect of ginger extracts and the principal components thereof (6-, 8- 10-gingerols and 6-, 8-, 10-shogaols) in an in vitro model. U937 cells, differentiated an exposed to lipopolysaccharide (LPS) from Escherichia coli (1 mg/ml). Extracts containing predominantly gingerols were found not to be cytotoxic, while shogaols were found to be cytotoxic at concentrations above 20 µg/ml (2007).
102. Jolad et al. also demonstrated the inhibitory effect of gingerols on LPS-induced PGE2 production in HL-60 cells stimulated with 1 µg/ml of LPS (2004). None of the compounds tested were shown to be cytotoxic.
Contaminants
103. Differences in cultivation conditions and extraction methods could lead to possible sources of contamination from toxins, microbes, pesticides, heavy metals and residual solvents. Studies investigating contamination in ginger are limited, however of the few available, the main sources of contamination reported are heavy metals (Wagesho & Chandravanshi, 2015; Goroya et al., 2019, Kilic & Soylak, 2019; Xu et al., 2020) and mycotoxins (Ałtyn and Twarużek, 2020; Wen et al., 2014; Omotayo et al., 2019; Lippolis et al., 2017).
104. Ginger can be exposed to mycotoxin contamination during harvesting, storage and handling. Whilst information on mycotoxin contamination in ginger is limited, ginger has been demonstrated to be particularly exposed to aflatoxins and ochratoxin A (OTA). This is reflected in GB legislation where maximum levels for spices including ginger are established in Retained EU Law 1881/2006. Maximum levels of 5 µg/kg for aflatoxin B1 (AFB1), 10 µg/kg for all aflatoxins (sum of AFB1, AFB2, AFG1, and AFG2) and 15 µg/kg for OTA, for ginger and its products.
105. The Committee discussed the potential presence of contaminants in ginger and noting that the ginger products used in the studies reported were sourced locally in markets or herbalists (Wagesho & Chandravanshi, 2015; Goroya et al., 2019), Members queried whether there were any specific data on contaminants in ginger supplements available in the UK.
106. The Committee noted it was unknown how much ginger and particularly, highly concentrated juice extracts, would contribute to overall contaminant exposure in the UK.
Annex A - Exposure
In this guide
In this guide107. TOX/2021/26 discussed exposure to ginger via the diet and in supplement form. TOX/2020/51 examined in more detail exposure to ginger in the form of highly concentrated juices (‘shots’). This statement reviews ginger from all sources described previously.
108. Many ginger supplements (Tables 1 and 2, Annex C) are recommended to support digestive and joint health, alleviate nausea, upset stomach, and travel sickness. Currently, a number of commercially available pregnancy supplements, including ‘Seven Seas Pregnancy’ and ‘Seven Seas Pregnancy Plus Follow On’, contain ginger extracts in their formulations.
109. The availability of supplements in different forms, along with a lack of information with regards to extraction processes involved and therefore composition of the extracts, meant it was not possible to consider aggregate exposures, as such, ginger exposure from the diet and supplements were separately considered.
110. In addition to supplements, pregnant women may also consume ginger as part of their general diet to various degrees. There are anecdotal reports of women using ginger products (Tables 3, Annex C) such as ginger biscuits and ginger ale, to alleviate morning sickness and nausea. Some may use these in combination with juice shots or tinctures (Table 4, Annex C).
111. Table 1 shows calculated exposures from the diet, supplements and drinks (including teas and shots). Mean acute ginger exposure from the diet of women aged 16-49 years old was 0.026 g/kg bw/day, and 97.5th percentile exposure was 0.16 g/kg bw/day. The corresponding mean and 97.5th percentile chronic exposures were 0.0083 and 0.058 g/kg bw/day, respectively. The upper value of the range of exposure from drinks and supplements was more than double (%) those estimated from 97.5th percentile acute exposure from the diet.
Table 1: Estimated mean and 97.5th percentile acute and chronic ginger exposures from a variety of sources in women aged 16 – 49 years old.
|
Source |
Range of daily exposures (g/day) |
Range of daily exposures (g/kg bw/day) |
Mean acute exposure* (g/day) |
Mean acute exposure* (g/kg bw/day) |
97.5th percentile acute exposure* (g/day) |
97.5th percentile acute exposure* (g/kg bw/day) |
Mean chronic exposure* (g/day) |
Mean chronic exposure* (g/kg bw/day) |
97.5th percentile chronic exposure* (g/day) |
97.5th percentile chronic exposure* g/kg bw/day |
|
Fooda |
No data |
No data |
1.7 |
0.026 |
11 |
0.16 |
0.55 |
0.0083 |
3.4 |
0.058 |
|
Drinks (Including tea and shots) b1,b |
0.5 - 32.5 |
0.0071 - 0.46 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
|
Supplements c |
0.010 - 24 |
0.00014 - 0.34 |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
No data |
1This assumes only one serving is consumed per day.
a Data obtained from the National Diet and Nutrition surveys years 1-8 calculated from women of a childbearing age (16-49 years) (Bates et al., 2014; 2016; Roberts et al., 2018)
b Data obtained online from retailers, see Appendix 1 for further details
c Data obtained online from retailers, see Appendix 1 for further details
*Rounded to 2 significant figures
112. As previously mentioned, 1 - 1.5 g per day may be advised during pregnancy (NHS, 2022, Healthline, 2020; Mother and baby, 2022). Some highly concentrated ginger shots commercially available contain up to 30 g of fresh ginger per serving, over 30 times that recommended by healthcare professionals.
113. As the NDNS does not provide data for pregnant women, there was uncertainty as to whether the data presented an accurate reflection of consumption during pregnancy. This uncertainty also extended to data presented for drinks and supplements, as the pattern of consumption during pregnancy to alleviate symptoms of sickness is unknown.
Annex A - Conclusions of the Committee
In this guide
In this guide114. Ginger is commonly used as a spice and flavouring in many countries worldwide and is increasingly growing in popularity as a natural remedy, due to its purported immune system-boosting properties, for easing motion sickness and post-operative nausea and vomiting, and pregnancy related nausea.
115. Several ginger supplements are commercially available, ranging from dried root in capsule form to tincture form, all with varying amounts of ginger. In addition to this, concentrated ginger shots, containing large amounts of pressed ginger, are increasingly becoming popular. The variability in the composition of these supplements adds uncertainty on the amount of ginger actually being consumed.
116. Study authors noted that some of the toxicity observed varied according to the nature of extraction solvent - organic solvent extracts exhibited more toxicity than aqueous extracts, which presumably indicates extraction of differentially toxic compounds. Hence, studies of individual extracts might not give the whole picture of the uncertainties involved.
117. Overall, the Committee concluded that based on the available information it was not possible to determine a point of departure to use in the risk assessment of ginger when used as a supplement.
118 Members noted that although the different ginger extracts were not comparable, there did appear to be some biological activity in the early stages of pregnancy. It was stressed that in general there was no indication of systemic toxicity from the use of ginger in the diet as food.
119. The lack of safety and toxicological information available on ginger use in pregnancy make it difficult to fully characterise the risks in this respect.
The committee noted that while there was some equivocal evidence for the possible effect of ginger on reproduction, it was not possible to characterise based on the data available.
120. Also, consumption data was based on women of childbearing age and therefore may not be representative of the maternal diet, leading to an under/overestimation of the actual exposure.
121. There is no clear indication that ginger is detrimental to pregnant women. Generally, normal levels of consumption of ginger within a diet is not considered a health concern. The Committee also noted that from the evidence presented, the potential for contamination of ginger with heavy metals and/or mycotoxins cannot be excluded.
COT Secretariat
December 2023
Annex A - References
In this guide
In this guideAlAskar, A; Shaheen, NA; Khan, AH; AlGhasham, N; Mendoza, MA; Matar, DB; Gmati, G; AlJeraisy, M; AlSuhaibani, A: (2020). Effect of daily ginger consumption on platelet aggregation. Journal of Herbal Medicine. Volume 20, 100316. https://doi.org/10.1016/j.hermed.2019.100316.
Alnaqeeb MA, Thomson M, Al-Qattan KK, Kamel F, Mustafa T, Ali M. (2003): Biochemical and histopathological toxicity of an aqueous extract of ginger. Kuwait J Sci Eng, 30: 35-48.
Al Omari, I; Afifi, F; Salhab, A. (2012). Therapeutic Effect and Possible Herb Drug Interactions of Ginger (Zingiber officinale Roscoe, Zingiberaceae) Crude Extract with Glibenclamide and Insulin. Pharmacognosy Communications. 2. 12-20. DOI:10.5530/pc.2012.1.4
Ałtyn, I., & Twarużek, M. (2020). Mycotoxin Contamination Concerns of Herbs and Medicinal Plants. Toxins, 12(3), 182. https://doi.org/10.3390/toxins12030182
The Committee on Toxicity of Chemicals in Food, Consumer Products and the environment (COT) (2020). Scoping Paper on Herbal Supplements Used in Pregnancy.
The Committee on Toxicity of Chemicals in Food, Consumer Products and the environment (COT) (2021). The potential effects that ginger and ginger supplements may have during pregnancy and lactation.
DTU Food Institute, (2019). The safety of pregnant women when ingesting ginger shots made from the root from real ginger (Zingiber officinale Roscoe). (Available in Danish only).
Dietz, Birgit & Hajirahimkhan, Atieh & Dunlap, Tareisha & Bolton, Judy. (2016). Botanicals and Their Bioactive Phytochemicals for Women's Health. Pharmacological reviews. 68. 1026-1073. Doi:10.1124/pr.115.010843
Egashira, K; Sasaki, H; Higuchi, S; Ieiri, I (2012). Food-drug Interaction of Tacrolimus with Pomelo, Ginger, and Turmeric Juice in Rats, Drug Metabolism and Pharmacokinetics, Vol 27, 2, 242-247. https://doi.org/10.2133/dmpk.DMPK-11-RG-105.
ElMazoudy, Reda & Attia, Azza. (2018). Phytomedicine. 50. 2018, 300-308, Ginger causes subfertility and abortifacient in mice by targeting both estrous cycle and blastocyst implantation without teratogenesis.
Ensiyeh, J.; Sakineh, M.A. (2009). Comparing ginger and vitamin b6 for the treatment of nausea and vomiting in pregnancy: A randomised controlled trial. Midwifery 2009, 25, 649–653. https://doi.org/10.1016/j.midw.2007.10.013
European Commission (EC) (2023). Commission Regulation (EU) 2023/915 of 25 April 2023 on maximum levels for certain contaminants in food and repealing Regulation (EC) No 1881/2006. Publications Office (europa.eu).
European Medicines Agency (2012): Assessment report on Zingiber Officinale Roscoe, rhizome; EMA/HMPC/577856/2010.
Finnish Food Authority, (2019). General Instructions on Safe Use of Foodstuffs.
Fischer-Rasmussen, W.; Kjaer, S.K.; Dahl, C.; Asping, U. (1991). Ginger treatment of hyperemesis gravidarum. Eur. J. Obstet. Gynecol. Reprod. Biol. 1991, 38, 19–24. https://doi.org/10.1016/0028-2243(91)90202-v.
Getaneh, A., Guadie, A., & Tefera, M. (2021). Levels of heavy metals in ginger (Zingiber officinale Roscoe) from selected districts of Central Gondar Zone, Ethiopia and associated health risk. Heliyon, 7(4), e06924. https://doi.org/10.1016/j.heliyon.2021.e06924
Goroya K, Mitiku Z, Asresahegn Y, (2019). Determination of concentration of heavy metals in ginger using flame atomic absorption spectroscopy. Afr. J. Plant Sci. 13, 163–167. DOI: 10.5897/AJPS2019.1787.
Healthline (2020). Ginger Tea in Pregnancy: Benefits, Safety, and Directions. Available at: Ginger Tea in Pregnancy: Benefits, Safety, and Directions (healthline.com).
Jiang, X., Williams, K. M., Liauw, W. S., Ammit, A. J., Roufogalis, B. D., Duke, C. C., Day, R. O., & McLachlan, A. J. (2005). Effect of ginkgo and ginger on the pharmacokinetics and pharmacodynamics of warfarin in healthy subjects. British journal of clinical pharmacology, 59(4), 425–432. https://doi.org/10.1111/j.1365-2125.2005.02322.x.
Kilic S, Soylak M (2020). J Food Sci Technol 57, 927–933 (2020). Determination of trace element contaminants in herbal teas using ICP-MS by different sample preparation method.
Kim, IS, Kim, SY, Yoo, HH (2012). Effects of an aqueous-ethanolic extract of ginger on cytochrome P450 enzyme-mediated drug metabolism. Die Pharmazie, 67(12), 1007–1009
Kimura Y, Ito H, Hatano T (2010). Effects of mace and nutmeg on human cytochrome P450 3A4 and 2C9 activity. Biol Pharm Bull. 2010;33(12):1977-82. doi: 10.1248/bpb.33.1977. PMID: 21139236.
Krüth P, Brosi E, Fux R, Mörike K, Gleiter CH (2004). Ginger-Associated Overanticoagulation by Phenprocoumon. Ann Pharmacother. Feb;38(2):257-60. doi: 10.1345/aph.1D225.
Lippolis V, Irurhe O, Porricelli, ACR, Cortese M, Schena R, Imafidon T, Oluwadun A, Pascale M (2017). Natural co-occurrence of aflatoxins and ochratoxin A in ginger (Zingiber officinale) from Nigeria. Food Control 2017, 73, 1061–1067.
Lumb A. B. (1994). Effect of dried ginger on human platelet function. Thrombosis and haemostasis, 71(1), 110–111. PMID: 8165628.
Mother and baby (2022) Available at: Ginger in pregnancy: Safety, benefits and guidelines (motherandbaby.com).
Mukkavilli, R., Gundala, S. R., Yang, C., Donthamsetty, S., Cantuaria, G., Jadhav, G. R., Vangala, S., Reid, M. D., & Aneja, R. (2014). Modulation of cytochrome P450 metabolism and transport across intestinal epithelial barrier by ginger biophenolics. PloS one, 9(9), e108386. https://doi.org/10.1371/journal.pone.0108386.
Nirmala, K., Prasanna Krishna T. and Polasa, K. (2007). In vivo Antimutagenic Potential of Ginger on Formation and Excretion of Urinary Mutagens in Rats. International Journal of Cancer Research, 3: 134-142. In vivo Antimutagenic Potential of Ginger on Formation and Excretion of Urinary Mutagens in Rats (scialert.net).
NICE (2021). Antenatal care. Management of nausea and vomiting in pregnancy. Available at: https://www.nice.org.uk/guidance/ng201/evidence/r-management-of-nausea-and-vomiting-in-pregnancy-pdf-331305934365
NHS (2021) Vomiting and morning sickness. Available at: Vomiting and morning sickness - NHS (www.nhs.uk) Accessed: 10/08/2023.
NHS (2021) Women and Health. Available at: Nausea and vomiting in pregnancy (wsh.nhs.uk).
NHS Specialist Pharmacy Service (2022). Herbal medicines: safety during pregnancy. Available at: Herbal medicines: safety during pregnancy – SPS - Specialist Pharmacy Service – The first stop for professional medicines advice.
Okonta JM, Uboh M, Obonga WO. (2008). Herb-drug interaction: a case study of effect of ginger on the pharmacokinetic of metronidazole in rabbit. Indian J Pharm Sci. 2008 Mar-Apr;70(2):230-2. doi: 10.4103/0250-474X.41462. PMID: 20046719; PMCID: PMC2792472.
Omotayo, O. P., Omotayo, A. O., Babalola, O. O., & Mwanza, M. (2019). Comparative study of aflatoxin contamination of winter and summer ginger from the North West Province of South Africa. Toxicology reports, 6, 489–495. https://doi.org/10.1016/j.toxrep.2019.05.011
Plengsuriyakarn, T.; Viyanant, V.; Eursitthichai, V.; Tesana, S.; Chaijaroenkul, W.; Itharat, A.; Na-Bangchang, K. (2012). Cytotoxicity, Toxicity, and Anticancer Activity of Zingiber Officinale Roscoe Against Cholangiocarcinoma, Asian Pacific Organization for Cancer Prevention, 13(9), pp. 4597–4606. doi: 10.7314/apjcp.2012.13.9.4597.
Portnoi, G., Chng, L. A., Karimi-Tabesh, L., Koren, G., Tan, M. P., & Einarson, A. (2003). Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. American Journal of Obstetrics and Gynecology, 189(5), 1374–1377. https://doi.org/10.1067/s0002-9378(03)00649-5
Rubin D, Patel V, Dietrich E. (2019). Effects of Oral Ginger Supplementation on the INR. Case Rep Med. Jun 11; 2019:8784029. doi:10.1155/2019/8784029. PMID: 31281366; PMCID: PMC6594244.
Smith, C; Crowther, C; Willson, K; Hotham, N; McMillian, V. (2004). A Randomized Controlled Trial of Ginger to Treat Nausea and Vomiting in Pregnancy. Obstetrics and Gynecology. 103. 639-45. DOI: 10.1097/01.AOG.0000118307.19798.ec.
Srivas K. C. (1984). Effects of aqueous extracts of onion, garlic and ginger on platelet aggregation and metabolism of arachidonic acid in the blood vascular system: in vitro study. Prostaglandins, leukotrienes, and medicine, 13(2), 227–235. https://doi.org/10.1016/0262-1746(84)90014-3
Srivastava KC (1986). Isolation and effects of some ginger components of platelet aggregation and eicosanoid biosynthesis. Prostaglandins Leukot Med. Dec;25(2-3): 187-98. doi: 10.1016/0262-1746(86)90065-x. PMID: 3103137.
Srivastava KC (1989). Effect of onion and ginger consumption on platelet thromboxane production in humans. Prostaglandins Leukot Essent Fatty Acids. Mar; 35(3):183-5. doi: 10.1016/0952-3278(89)90122-1 PMID: 2710801.
Stanisiere, J., Mousset, P. Y., & Lafay, S. (2018). How Safe Is Ginger Rhizome for Decreasing Nausea and Vomiting in Women during Early Pregnancy? Foods (Basel, Switzerland), 7(4), 50. https://doi.org/10.3390/foods7040050
Thomson M, Al-Qattan KK, Al-Sawan SM, Alnaqeeb MA, Khan I, Ali M (2002). The use of ginger (Zingiber officinale Rosc.) as a potential anti-inflammatory and antithrombotic agent. Prostaglandins Leukot Essent Fatty Acids. Dec; 67(6):475-8. DOI: 10.1054/plef.2002.0441. PMID: 12468270.
Tiran, D. (2012). Ginger to reduce nausea and vomiting during pregnancy: Evidence
of effectiveness is not the same as proof of safety. Complementary Therapies in Clinical Practice 18 (2012) 22-25.
Vutyavanich T, Kraisarin T, Ruangsri R. (2001). Ginger for nausea and vomiting in pregnancy: randomized, double-masked, placebo-controlled trial. Obstet Gynecol. 2001 Apr;97(4): 577-82. DOI: 10.1016/s0029-7844(00)01228-x. PMID: 11275030.
Wagesho Y, Chandravanshi BS, (2015). Levels of essential and non-essential metals in ginger (Zingiber officinale) cultivated in Ethiopia. SpringerPlus 4, 1–13. Doi: https://doi.org/10.1186/s40064-015-0899-5.
Wen J, Kong W, Hu Y, Wang J, Yang M (2014). Multi-Mycotoxins analysis in ginger and related products by UHPLC-FLR detection and LC-MS/MS confirmation. Food Control 2014, 43, 82–87. doi: 10.1016/j.foodcont.2014.02.038.
Willetts KE, Ekangaki A, Eden JA. (2003). Effect of a ginger extract on pregnancy-induced nausea: a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2003 Apr;43(2):139-44. doi: 10.1046/j.0004-8666.2003.00039.x. PMID: 14712970.
Xu J, Zhang J, Lv Y, Xu K, Lu S, Xiaohui Liu, Yang Y, (2020). Effect of soil mercury pollution on ginger (Zingiber officinale Roscoe): Growth, product quality, health risks and silicon mitigation. Ecotoxicology and Environmental Safety, Volume 195, 2020, 110472, ISSN 0147-6513. https://doi.org/10.1016/j.ecoenv.2020.110472
Young HY, Liao JC, Chang YS, Luo YL, Lu MC, Peng WH (2006). Synergistic effect of ginger and nifedipine on human platelet aggregation: a study in hypertensive patients and normal volunteers. The American Journal of Chinese Medicine. 34(4):545-551. DOI: 10.1142/s0192415x06004089
Yu, Y., Zick, S., Li, X., Zou, P., Wright, B., & Sun, D. (2011). Examination of the pharmacokinetics of active ingredients of ginger in humans. The AAPS journal, 13(3), 417–426. https://doi.org/10.1208/s12248-011-9286-5.
Verma, S. K., Singh, J., Khamesra, R., & Bordia, A. (1993). Effect of ginger on platelet aggregation in man. The Indian journal of medical research, 98, 240–242.
Zaeoung, S.; Plubrukarn, A.; Keawpradub, N. (2005) Cytotoxic and free radical scavenging activities of zingiberaceous rhizomes. Songklanakarin J. Sci. Technol. 2005, 27, 799–812.
Annex B - Summary of Studies
In this guide
In this guideHuman Studies
|
Author/Date |
Study type |
Study size/No. of Patients at End |
Exposure (ginger dose/day) |
Study period |
Length of Treatment (days) |
Main outcome measures |
Main results |
|
Chittumma et al., 2007 |
Randomized double-blind controlled trial. |
126/123 |
Ginger powder |
4 days |
4 |
Change in nausea and vomiting scores (3 symptoms on Rhodes index); |
Results showed that ginger is |
|
Ensiyeh et al., 2005 |
Double-blind randomised controlled trial. |
70/69 |
Ginger powder |
3 months |
4 |
Severity of nausea (VAS 0–10); number of vomiting episodes; general response to treatment (5-item Likert scale); occurrence of side-effects or adverse |
two spontaneous abortions in ginger group, 1 in B6 group; no congenital anomalies observed in babies brough to term. |
|
Fischer-Rassmussen et al., 1991 |
Double-blind randomised crossover trial |
30/27 |
Ginger powder |
11 days |
4 |
Preference of treatment period; relief scores (4-point scoring system); outcome of pregnancy |
One spontaneous abortion, One elected. No adverse effects were observed in remaining 25 subjects. |
|
Portnoi, 2003 |
Not specified |
187 pregnant women |
Various, not specified |
up to 12 months post birth |
Minimum of 3 days |
Safety and effectiveness of ginger for nausea and vomiting of pregnancy (NVP). |
Three major malformations were reported in the ginger group, ventricular septal defect (VSD), right lung abnormality, and kidney abnormality (pelviectasis). One incidence of idiopathic central precocious puberty at age 2 years. No significant difference between the two groups in terms of live births, spontaneous abortions, stillbirths, therapeutic abortions, birth weight, or gestational age |
|
Smith, 2004 |
Randomized, controlled equivalence trial |
291 women, less than 16 weeks pregnant |
1.05 g ginger |
3 weeks |
3 weeks |
Ginger verses B6 for the treatment of nausea or vomiting in pregnancy |
Three spontaneous abortions in ginger group, 9 abortions in B6 group |
|
Vutyavanich, 2001 |
Double blind |
32 |
Ginger powder |
5 months |
4 |
Severity of nausea (VAS 0–10); number of vomiting episodes; general response to treatment after 1 week (5-item Likert |
Ginger was significantly more effective than the placebo in relieving the severity of nausea in pregnancy (p = 0.014). |
|
Willetts et al., 2003 |
Double-blind randomised placebo-controlled trial |
120/99 |
Ginger extract |
8 months |
4 |
Used RINVR to measure frequency, duration, distress caused by nausea, vomiting and retching; long term follow-up for birth outcome |
Three spontaneous abortions observed in ginger group |
Human studies – Platelet Aggregation
|
Author/date |
Study design |
Population/stud size |
Study Duration |
Exposure |
Outcome |
Results |
Comment |
|
Bordia |
Placebo controlled |
Patients with |
3 months. Outcomes |
Dose: 4g per day Unstandardised |
Platelet aggregation— |
Ginger had no |
Ginger had no significant effect on blood lipids or blood sugar. |
|
Bordia |
No data. |
No data. |
No data. |
No data. |
Fibrinogen; |
No data. |
No mention of |
|
Bordia |
No data. |
No data. |
No data. |
No data. |
Fibrinolytic activity |
No data. |
P value not reported |
|
Bordia |
No data. |
20 |
1 day. Outcomes |
10 g single dose. Unstandardised capsules |
Platelet aggregation. - Agonist(s): ADP and Epi |
Reduction of both |
No data. |
|
Jiang et al., |
Randomized, |
Healthy male |
Total study period: |
Dose: 3.6g (3x 0.4g, 3x per day) Unstandardized |
Platelet aggregation, Agonist: AA; INR; Plasma warfarin |
No significant |
P value not reported |
|
Lumb. |
Randomised, |
Healthy male |
Total study period: |
Dose: 2g (4 x 500 mg) dried ginger per day Unstandardized |
Platelet aggregation; - Agonist(s): AA, ADP, collagen, ristocetin, ADP; Bleeding time; Platelet count; Thromboelastography |
No significant |
No data. |
|
Rubin et al., 2019 |
Case report |
Female, 70 yrs |
No data. |
48 mg daily Chewable ginger supplement for approx. 1 month |
INR - 8.0 approx. 1 month after taking ginger supplement. |
INR reduced to 2.6 following cessation of ginger supplementation and pause in warfarin administration
|
Patient also taking clonazepam 1 mg,
|
|
Srivastava |
Open-label |
Healthy female |
Total study period: 7 |
Dose: 5g raw ginger |
Platelet thromboxane B2 production |
Ginger consumption |
No data. |
|
Verma |
Randomised |
Healthy male |
Total study period: |
Dose: 5g (4 x 625 mg, twice per day); dry ginger powder - Unstandardized |
Platelet aggregation. Agonist(s): ADP and Epi |
Ginger significantly |
Platelet aggregation |
|
Young et al., 2006 |
Not specified |
20 |
72 days |
1 g ginger (+ 10 mg nifedipine) |
Synergistic effect of ginger and nifedipine on anti-platelet aggregation in normal human volunteers and hypertensive patients. |
Ginger and nifedipine had synergistic |
No data. |
In vitro studies
|
Author |
Test System |
Exposure |
Characterisation of test substance |
Main outcome measure |
Outcome |
|
Abudayyak et al., 2015 |
Ames: Salmonella typhimurium TA98 and TA100 strains; Cytotoxicity assay: Rat kidney NRK-52E cell line |
Cytotoxicity assay: (0.75, 1.50, 3.00, 6.00, 12.00, |
Aq, chloroform and MeOH ginger extracts |
Cytotoxicity and genotoxicity |
Chloroform extract cytotoxic: IC50 = 9.08 mg/ml; aqueous extract mutagenic at all concentrations against T98 strain, in presence of S9 mix |
|
Mohammed et al., 2016 |
chick embryonic heart micromass; mouse D3 embryonic stem cell systems (ESD3) |
0.75–100 uM Micromass assay: 6 days, ESD3: 12 days |
6-gingerol |
Embryotoxicity |
no significant changes in contractile and cellular activity or changes in total protein content in 6-gingerol-treated primary embryonic chick cardiomyocytes. |
|
No data. |
No data. |
No data. |
No data. |
No data. |
inhibition in contractile activity at 12.5–50 μM |
|
No data. |
No data. |
No data. |
No data. |
No data. |
Change in both cellular activity and protein content in a dose-dependent manner at high concs (12.5–100 μM) |
|
No data. |
No data. |
No data. |
No data. |
No data. |
Significant decrease in cardiomyocyte differentiation for all tested concentrations except 0.75 μM in ESD3 |
|
No data. |
No data. |
No data. |
No data. |
No data. |
Significant decrease in cellular activity and protein content of stem cell-derived cardiomyocytes with increased 6-gingerol concentration exposure. |
|
Nakamura & Yamamoto (1982) |
Escherichia coli Hs30 |
Not specified |
Juice of ginger rhizome, 6-gingerol |
Mutagenicity |
ginger juice supressed spontaneous mutation; 6-gingerol mutagenic in isolation |
|
Nakamura & Yamamoto 1983 |
Escherichia coli Hs30 |
Not specified |
6-shogaol, 6-gingerol |
Mutagenicity |
[6]-Shogaol was 104 times less |
|
Nirmala et al., 2007 |
Wistar rats, male |
Salmonella typhimurium strains TA 98 and TA 100 |
Ginger paste and powder, unboiled, boiled, unfried, fried Ames test: Ginger paste: 1, 2 and 3 mg; powder: 0.5, 1 and 1.5 g |
Anti-mutagenicity |
Anti-mutagenic potential unaltered by treatment of ginger.
|
|
Plengsuriyakarn et al., 2012 |
Cholangiocarcinoma (CCA) cell line 6 (CL-6), hepatocarcinoma (HepG2) and normal human renal epithelium (HRE) |
1.95, 3.90, 7.81, 15.62, 31.25, 62.5, 125, and 250 µg/ml |
Crude ethanolic ginger extract |
Cytotoxicity |
IC50 and cytotoxicity 10.95 and 53.15, μg/ml |
|
Sivaswami et al., 1991 (Abstract) |
Salmonella typhimurium strains TA 98, TA 100 and TA 1535 |
Unknown |
Essential oil from ginger |
Mutagenicity |
Non mutagenic |
|
Soudamini et al., 1995 |
Salmonella typhimurium strains TA 100, 98 |
25 and 50 mg/plate |
ethanolic mixture of powdered ginger |
Mutagenicity |
mutagenicity in both TA 1535 and TA 100 at both concentrations |
|
Zaeoung et al., 2005 |
breast (MCF7) and colon (LS174T) cell lines |
Not specified |
aqueous extract and volatile oils |
Cytotoxicity |
IC50 > 39.2 μg/ml |
In vivo studies
|
Author |
Test System |
Study size |
Exposure |
Characterisation of test substance |
Duration |
Main outcome measure |
Outcome |
|
Alnaqeeb et al., 2003 (abstract) |
Rats, female |
Unknown |
Oral and intraperitoneal. 50 mg/kg and 500 mg/kg |
Aqueous ginger extract |
28 days |
No data. |
Increased levels of serum aspartate aminotransferase (AST) and decreased levels of alanine aminotransferase (ALT) in orally dosed rats |
|
Dissabandara & Chandrasekara, 2007 |
Sprague-Dawley rats |
15 in 3 groups, otherwise not specified |
Oral: 500 mg/kg/day and 1000 mg/kg/day during days 5 to 15 of gestation |
Powdered ginger extract |
Animals treated with ginger for 10 days |
Effect of powdered ginger extract administered prenatally on postnatal development |
Lower intake of food and water and lower weight gain in ginger treated group |
|
ElMazoudy and Attia, 2018 (abstract only) |
ICR mice |
Unknown |
250, 500, 1000, or 2000 mg/kg bw/d aqueous ginger extract. |
Powdered dried ginger root |
35-day treatment study; 20 day study (antifertility and abortifacient loss) |
Effect on oestrus cycle and implantation in female mice. |
Female copulation index was significantly reduced at 2000 and 1000 mg/kg bw/d groups; female pregnancy index significantly decreased at the highest dose. No. of implantation sites and live fetuses in the 2000 mg/kg bw/d group lower than the other treated and control groups. |
|
Hosseini et al., 2015 (abstract only) |
Rats, female and male offspring |
72 (groups of 9) |
Oral: 50, 100 and 200 mg/kg bw during neonatal and perinatal periods |
Alcoholic ginger extract |
Unknown |
Serum testosterone, LH and FSH. Effect on spermatogenic cell lines in male mature offspring rats |
Significant increase in testosterone levels and number of spermatogenic cells. Significant reduction in FSH and LH at doses of 100 and 200 mg/kg bw compared to control |
|
Jeena et al., 2011 |
Wistar rat |
30 |
Oral: 100, 250, and 500 mg/kg per day once daily |
Ginger essential oil |
13 weeks |
Oral Toxicity |
No mortaility or abnormal changes observed in relative organ weights w.r.t. body weight. Increase in serum Na levels in male rats treated with 500 mg/kg/d. slight increase in total bilirubin in female rats, along with a decrease in AST and ALT levels. No significant changes in hepatic function parameters (alkaline phosphatase, total protein, albumin and globulin content). |
|
Malik and Sharma, 2011 |
Wistar rat, male |
Not specified |
gastric gavage: 250, 500 and 1000 mg/kg, (corresponding to 5, 10 and 20% of the NOAEL of the lyophilised ginger powder (5000 mg/kg) |
Lyophilsed ginger juice powder |
Experiment 2: 8 weeks. Exp 1&2 not specified |
Acute Toxicity |
no signs of toxicity or mortality |
|
Plengsuriyakarn et al., 2012 |
OV and nitrosamine (OV/ |
90 |
1000, 3000, and 5000 mg/kg bw/d |
No data. |
30 days |
Acute Toxicity |
No data. |
|
Rong et al., 2009 |
Sprague–Dawley rats, male and Female |
40 |
Gavage: 500, 1000 and 2000 mg/kg bw/day |
Powdered Japanese ginger, |
37 |
35 day repeat dose |
No increase in mortality. Slightly reduced absolute and relative weights of testes (by 14.4% and 11.5%, respectively) at highest dose. |
|
Shalaby and Hamowieh, 2010 |
Sprague Dawley rats, |
120 |
Oral, 5 to 17.5 g/kg bw |
water or methanolic ginger extract |
65 days |
Fertility, serum testosterone and acute toxicity |
oral Lethal Doses (LD50) of the methanolic and water extracts - 10.25 and 11.75 g/kg bw respectively. No symptoms of toxicity observed at doses up to 5 g/kg bw. Both extracts increased fertility index, sexual organ weight, and sperm motility and count after 65 consecutive days |
|
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
Methanolic extract: Testosterone levels increased to 4.08 ± 0.10 and 7.13 ± 0.14 ng/dL (both significant at P < 0.001); Water extract (150 and 300 mg/kg bw): Serum testosterone levels increased 4.06 ± 0.03 and 5.04 ± 0.08 ng/dL (both significant at P < 0.001) |
|
No data. |
No data. |
No data. |
100 and 200 mg/kg bw for 65 consecutive days and water extracts at doses of 150 and 300 mg/kg bw |
No data. |
No data. |
Fertility Index |
Mild to moderate degenerative changes of spermatogenic cells, diffuse oedema and incomplete arrest of spermatogenesis. Mild degeneration of spermatogenic cells and slight oedema of interstitial cells in testes of rats orally administered 300 mg/kg bw water extract. LOAEL of 200 mg/kg bw/day for the methanolic extract suggested |
|
Weidner & Sigwart, 2001 |
Wistar rats, pregnant female |
176 (88 Females) |
Gastric intubation: 100, 333 and 1000 mg/kg from days 6-15 |
EV.EXT 33, a patented Zingiber officinale extract (comprising 6-gingerol, 8-gingerol, 10-gingerol, 6-shogaol, and 8-shogaol (1.9 w/w of the extract)) |
21 days |
teratogenicity |
No maternal or developmental toxicity observed |
|
Wilkinson 2000 |
Sprague-Dawley rats, F |
43 |
Oral, drinking water on days 6-15 |
20 g/L or 50 g/L ginger tea |
20 days |
Reproductive and developmental toxicity |
Embryonic loss in the treated groups 2x that of the controls. Exposed foetuses found to be significantly heavier than control. No gross structural malformations observed |
Effect on CYPs and prostaglandin activity
|
Author |
Test System |
Exposure |
Characterisation of test substance |
Main outcome measure |
Outcome |
|
Dugasani et al., 2010 |
Mouse leukaemic monocyte (RAW 264.7) |
1, 3 and 6 uM |
[6]-gingerol, [8]-gingerol, [10]-gingerol |
Compare the antioxidant and antiinflammatory |
Dose dependant inhibition of activated PGE2 release. Inhibition reached 58, 66, 73 |
|
Jolad et al., 2004 |
HL-60 cells |
Not specified |
Ginger constituents: gingerols, shogaols, 3-dihydroshogaols, gingerdiols |
Effects of ginger components on LPS-induced PGE2 production |
No cytotoxicity demonstrated |
|
Jolad et al., 2005 |
HL-60 cells |
Not specified |
Ginger constituents conatining gingerols, shogaols, 3-dihydroshogaols, gingerdiols |
Effects of ginger components on LPS-induced PGE2 production |
Inhibition of LPS-stimulated |
|
Kim et al., 2012 |
Human liver microsomes |
0.05–5 ug/ml |
Aqueous ethanolic ginger |
Inhibitory effect on CYP450-mediated drug metabolism |
Concentration-dependent |
|
Kimura et al., 2010; |
Human CYP3A4 and |
Not specified |
Inhibitory effect on CYP3A4 and CYP2C9 activity |
significant inhibition of CYP3A4 IC50 5.1u g/ml or CYP2C9 IC50 (10ug/ml) activity |
|
|
Lantz et al., 2007 |
U937 cells |
0.1 ug/ml for 6 hrs |
Ginger extract and mixtures of 6-, 8- 10-gingerols and 6-, 8-, 10-shogaols |
Effect on inflammatory |
No effect on COX-2 expression |
|
Mukkavilli et al., 2014 |
Human liver microsomes |
Ginger extract: 500 mg/ml (containing 15 mg/ |
Ginger extract: (containing 6-Gingerol, 8-Gingerol, 10-Gingerol, 6-Shogaol). All |
Effect of ginger extract and major |
Inhibition of CYP1A2 (IC50 - |
Effect on Platelet Aggregation
|
Author |
Test System |
Study size |
Exposure |
Characterisation of test substance |
Main outcome measure |
Outcome |
|
Srivas, 1984 |
Human platelets and rat aorta |
No data. |
15-20 ul (concentrations not given) |
Ginger extracts in water, n-hexane, chloroform, and ethyl acetate |
Effect of ginger extracts on in vitro platelet aggregation |
Inhibition of arachidonic acid (AA), epinephrine, adenosine diphosphate (ADP), and collagen-induced platelet aggregation |
|
Srivastava, 1986 |
Platelet rich plasma (no further information given) |
No data. |
10-20 ul (concentrations not given) |
No data. |
Effect of ginger and components on platelet aggregation and eicosanoid biosynthesis |
Reduced thromboxane formation from exogenous AA; Inhibition of AA, epinephrine, ADP and collagen-induced platelet aggregation |
|
Srivastava |
Open-label |
Healthy female |
Total study period: 7 |
Dose: 5g raw ginger |
Platelet thromboxane B2 production |
Ginger consumption |
|
Suekawa et al., 1986 (abstract only) |
Rat hind paw and aorta, rabbits |
Unknown |
Unknown |
6-shogaol |
Effect of 6-shogaol on arachidonic acid cascade |
Inhibition of carrageenin-induced swelling of hind paw in rats and arachidonic acid (AA)-induced platelet aggregation in rabbits. Inhibition of prostaglandin 12 (PGI2) release in rat aorta. Possibly caused by COX inhibition |
|
Thomson et al., 2002 |
Sprague-Dawley rats, Adult, F; ex vivo |
36 |
50 mg/kg or 500 mg/kg daily by gavage or intraperitoneally (IP) for 4 weeks |
Aqueous ginger extract, equivalent of 500 mg/ml |
ex vivo effect |
Serum PGE2 reduced and both dose levels; high dose significantly reduced serum TXB2 both orally and IP; A non-significant reduction in the level of |
|
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
Significant reduction in levels of |
Herb-drug interactions
|
Author |
Test System |
Study size |
Exposure |
Characterisation of test substance |
Duration |
Main outcome measure |
Outcome |
|
Al-Omari et al., 2012 |
Albino rat, M |
30: 5 groups of 6; 72: 12 groups of 6; |
25, 50 and 100 mg/kg bw by gavage; single dose (50 mg/kg bw)and up to one week |
Ginger crude extract |
Multiple dose: 2 weeks; single dose: 1 week |
Effect on glibenclamide and insulin; hypoglycaemic and antihyperglycemic effects in normoglycemic- and streptozotocin-induced (STZ) diabetic rats |
Significant decrease in blood glucose level (BGL) in normoglycemic rats after 1 & 2 hrs (50 mg/kg). Significant decrease in non-fasting BGL (N-FBGL) in STZ- diabetic rats |
|
Egashira et al., 2012 |
Sprague-Dawley rat, M (7 weeks old) |
Not specified |
10 mL/kg orally |
50% ginger juice |
1-3 days |
interaction between ginger juice and tacrolimus |
Significant increase in tacrolimus blood concentrations in rats treated with ginger juice, compared to those treated with water or orange juice |
|
Okonta et al., 2008 |
Rabbits (3F, 2M) |
5 |
1 ml/kg, orally |
Ginger extract |
3 days |
Effect of ginger on the pharmacokinetics of metronidazole |
Significant increase in absorption and plasma half-life; significant decrease in the elimination rate constant and clearance of metronidazole. |
Annex C - Assessment of Exposure
In this guide
In this guide1. The relative proportions of the active components of ginger – gingerols, shogaols and curcumin occur in varying proportions, depending on the variety of rhizome and the area of cultivation.
2. Many ginger supplements (Tables 1 and 2) are recommended to support digestive and joint health, alleviate nausea, upset stomach, and travel sickness. Currently, two commercially available pregnancy supplements – ‘Seven Seas Pregnancy’ and ‘Seven Seas Pregnancy Plus Follow On’ – contain 10 mg ginger extract.
Table 1. Sample of ginger supplements in capsule and tablet form commercially available.
|
Commercial Product Name |
Form |
Composition |
Daily dose recommended by vendor or website |
|
Seven Seas Pregnancy |
Tablet |
Ginger extract 10 mg |
1 tablet a day. |
|
Seven Seas Pregnancy Plus Follow-On |
Tablet, capsule |
Ginger extract 10 mg |
One tablet and one capsule/ day |
|
Supplemented |
Tablet |
Ginger Extract 3,000 mg (20:1) |
1-2 tablets daily |
|
Good n Natural |
Capsule |
Powdered root 550 mg |
2 capsules daily |
|
Woods Supplements |
Tablet |
Ginger extract 500 mg |
1 tablet daily |
|
Solgar |
Capsules |
Ginger (Zingiber officinale) Root Powder 150 mg, Standardised Ginger (Zingiber officinale) Root Powdered Extract (5% ginger gingerols) 300 mg |
1-2 capsules daily |
|
Solgar |
Capsules |
Ginger (Zingiber officinale) Root Powder 500 mg. Ginger (Zingiber officinale) Root Powdered Extract (4:1) 5 mg. |
1-3 capsules daily |
|
Swanson |
Capsules |
Ginger Root 540 mg |
2 capsules daily |
|
Bio Health |
Capsules |
Ginger Root 500 mg |
No data. |
|
Biovea |
Capsules |
Ginger (root) (std. to 5% gingerols, 12.5 mg) 250 mg |
1-3 daily |
|
Jarrow Formulas |
Capsules |
Ginger root (concentrate) (Zingiber officinale) 500 mg |
1 daily |
|
Nature’s Best |
Capsule |
Ginger Root 14,400 mg (provided by 120 mg of a 120:1 extract) providing 24 mg gingerols |
1 daily |
|
NeuLife |
Tablets |
Ginger Extract 12000 mg |
1-2 tablets daily |
|
Lifeplan |
Capsule |
Ginger 12:1 Extract |
1-2 tablets daily |
|
ALPHA01 |
Capsules |
Ginger root powder 1100 mg |
2 capsules daily |
|
|
Tablet |
Ginger Extract 12,000 mg (20:1) standardised to 600mg 12,000 mg |
1-2 tablets daily |
|
Now Foods Capsules Superfood World |
Capsules |
Ginger Extract (Zingiber officinale) (Root) (Standardized to min. 5% Gingerols) 250 mg: Ginger Powder (Zingiber officinale) (Root) 225 mg |
1-3 capsules daily |
|
Viridian Ginger |
Capsules |
One vegetarian capsule provides: Certified organic Ginger root 400 mg |
1-3 capsules daily |
Table 2: Sample of ginger supplements in liquid and powder forms commercially available
|
Commercial Product Name |
Form |
Composition |
Daily dose recommended by vendor or website |
|
Indigo Herbs |
Tincture |
Zingiber officinale, Alcohol, Water. Extraction Ratio: 1:3, Alcohol Volume: 25% |
1-2 ml, 2-3 times Daily 20 drops from the glass dropper equals ~ 1ml |
|
Nature’s Answer |
Tincture |
Ginger (Zingiber officinale) root extract: 145 mg |
1 ml (28 drops) three times per day |
|
Herb Pharm |
Tincture |
Ginger rhizome (Zingiber officinale) extract 598 mg (Extraction rate 140 mg herb per 0.7 ml) |
“1 full squeeze of the dropper bulb to 2 oz. of water or juice, 2 - 5 times per day. |
|
Indigo Herbs |
Powder |
100% Pure Zingiber officinale Powder |
1/3 teaspoon powder in water 3 times a day. (1 tsp = 3g) |
|
Organic Herbal Remedies |
Tincture |
herb to pure grain alcohol of 1:3. 1ml is the equivalent of 333mg of dried ginger root. W |
0.2ml to 0.4ml three times a da in a little water. Children 6-12 years old 0.1ml to 0.2ml three times a day |
|
Biovea |
Tincture |
Fresh Organic Ginger (root) (667 mg per 1 ml serving) |
30 drops (~ 1 ml), 1-3 times daily or as needed |
|
Epigenar
|
Tincture |
Purified water, organic alcohol, organic ginger (Zingiber officinale) (amounts not specified) |
15 drops, 3 times daily Max 60 drops per day unless otherwise advised. Children aged 4-15 years, 3 times daily, one drop per number of years of age. |
Consideration of ginger from other sources
3. In addition to supplements, pregnant women may also consume ginger as part of their general diet to various degrees. There are anecdotal reports of women using ginger products such as ginger biscuits and ginger ale, to alleviate morning sickness and nausea. Some may use these in combination with juice shots or tinctures.
Table 3: Sample of ginger-containing foods commercially available.
|
Commercial product name |
Form |
Composition |
|
Border Biscuits Dark Chocolate & Ginger |
Ground ginger |
Ground ginger 1.5 % |
|
Sainsbury's Stem Ginger Cookies, Taste the Difference |
Stem ginger |
Candied Stem Ginger (17%) (Australian Stem Ginger, Sugar); ginger powder |
|
Sainsbury's Dark Chocolate & Ginger Cookies, Taste the Difference |
Stem ginger |
Candied Stem Ginger (13%) (Australian Stem Ginger, Sugar); ginger powder |
|
Nairn's Wheat Free, Ginger Biscuits |
Stem ginger |
Stem Ginger (6.4%) (Stem Ginger, Sugar); Ground Ginger |
|
Sainsbury's Ginger Nut Biscuits, SO Organic |
Powdered ginger |
Ginger Powder (0.6%) |
|
Nooro Lemon + Ginger CBD Bar |
No data. |
Ginger (0.5%), |
|
Rhythm 108 Lemon, Ginger & Chia Biscuit Share Bag |
Dried ginger powder |
Organic gluten free oat flour (33%), organic coconut oil (24%), organic coconut flower sugar, organic almonds, organic chia seeds (5%), organic lemon zest (1.3%), organic lemon oil, organic ginger powder (0.4%), |
Table 4: Ginger containing teas, juices and drinks commercially available.
|
Commercial Product Name |
Form |
Composition |
|
Gimber |
Liquid concentrate |
38% organic and high-quality ginger, organic lemons, herbs and spices |
|
Moju |
liquid |
Apple, Ginger Root (25%), Lemon, Antioxidant: Ascorbic Acid |
|
James White Drinks Organic Ginger Zinger Shot 70ml |
liquid |
Organic Apple Juice (73%), Organic Ginger Juice (27%), Water, Antioxidant: Ascorbic Acid |
|
James White Drinks Organic Xtra Ginger Zinger Shot 70ml |
liquid |
Organic Apple Juice (59.5%), Organic Ginger Juice (40%), Organic Chilli Flavouring (0.5%), Antioxidant: Ascorbic Acid |
|
Twinings Lemon & Ginger Tea |
Tea |
Ginger Root* (37%), Natural Lemon Flavouring with Other Natural Flavourings (25%), Lemongrass*, Blackberry leaves*, Lemon Peel, Sweet Fennel*, Natural Ginger Flavouring with Other Natural Flavourings (3.5%), |
|
Pukka Organic Ginger, Galangal & Golden Turmeric Tea |
Tea |
Ginger Root (52%) |
|
Belvoir Ginger Cordial |
No Data. |
Pressed Ginger Juice 2%, Ginger Extracts, |
|
Old Jamaica Ginger Beer |
Drink |
Ginger root extract |
|
Fever Tree Ginger Beer Light |
Drink |
Ginger Root, Natural Ginger Flavouring with other Natural Flavourings |
|
Fentimans Ginger Beer
|
Drink |
Fermented Ginger Root Extract (Water, Glucose Syrup, Ginger Root, Pear Juice Concentrate, Yeast); Natural Flavourings (Ginger, Lemon, Capsicum) |
|
Cawston Press Apple & Ginger Juice |
Juice |
1% Ginger Extract |
|
Pukka Lemon Ginger & Manuka Tea |
Tea |
Ginger Root (32%) |
|
Twinings Spiced Ginger Tea |
Tea |
Ginger Root* (70%), Liquorice Root* (15%), Cinnamon* (10%), Cloves* (5%) |
|
No.1 Kombucha Ginger & Turmeric |
Tea drink |
Kombucha (Filtered Water, Cane Sugar*, Green Tea*, Live Kombucha Cultures), Ginger Juice* (1.5%), Ginger* (0.14%), Turmeric* (0.14%), Black Pepper* |
|
Teapigs Lemon & Ginger Tea Bags |
Tea |
Ginger (65%), Lemongrass, Lemon Peel (5%), Liquorice Root |
|
MOJU Ginger Juice Shot 60ml |
Juice |
17.2g fresh ginger root'. Apple, Ginger Root (25%), Lemon, Antioxidant: Ascorbic Acid |
|
Innocent Shots Ginger Kick, Kicking Ginger & Spicy Turmeric 100ml |
Juice shot |
Apple Juice (54%), Carrot Juice (15%), Ginger Juice (10%), Red Pepper Juice, Lemon Juice, Orange Juice, Jalapeño Pepper Juice, Turmeric Juice (0.2%), Vitamin D |
|
Plenish Organic Ginger Immunity Juice Shot |
Juice shot |
Apple, Ginger (20%), Lemon, Apple Cider Vinegar (7%), Acerola Cherry Powder |
|
Lo Bros Organic Kombucha Gut Shot Ginger |
Juice shot |
Carrot Juice* (30%), Orange Juice*, Ginger Juice* (25%), Kombucha (14%) (Filtered Water, Kombucha Culture*, Green Tea*, Oolong Tea*, Raw Sugar*), Lemon Juice Concentrate", Living Cultures |
|
Belvoir Ginger Beer |
Drink |
Carbonated Spring Water, Sugar, Lemon Juice from Concentrate, Fresh Root Ginger Infusion 2%, Pressed Ginger Juice, Ginger Extracts, Lemon Extract, Capsicum Extract |
|
Grace Tropical Rhythms Sorrell Ginger |
Drink |
Water, Sorrel Cordial (Water, Sugar, Sorrel Flower (3%), Acid: Citric Acid), Rum Flavouring, Natural Sorrel Powder (0.13%), Ginger Emulsion (Water, Ginger Flavouring (.006%), Acid: Citric Acid, Capsicum, Stabilisers: Acacia Gum, Ester Gum), Colour: E129 |
Background Exposure from the diet
Exposure estimates based on the NDNS
4. Table 5 provides exposure estimates for women of childbearing age (16 - 49 years) from years 1 – 8 of the NDNS survey (Bates et al., 2014; 2016; Roberts et al., 2018). The NDNS (Bates et al., 2014; 2016; Roberts et al., 2018) does not provide data for pregnant or lactating women so while data is based on women of childbearing age, this data may not necessarily be representative of the maternal diet. The food group used for the exposure assessment consisted of all foods within the NDNS database which contained ginger (raw, powdered etc) except for alcoholic beverages. Mean chronic ginger exposure from the diet of women aged 16 - 49 years old was 0.0083 g/kg bw/day, and at a 97.5th percentile consumption was 0.058 g/kg bw/day.
5. Table 5 indicates the contribution of ginger to the diet of women aged 16-49 years is low, therefore, the main contributor to exposure for some could be from supplement use. This may vary however according to country of origin. For example, ginger is used more and in larger quantities in foods in Asian, African and Caribbean communities.
6. The NDNS does not provide data for pregnant women, therefore there would be uncertainty as to whether this give an accurate reflection of exposure during pregnancy, especially in women who will use ginger drinks and teas or foods such as ginger biscuits to alleviate symptoms of pregnancy associated sickness.
7. TOX/2021/26 demonstrated that the potential risks arising from exposure to ginger from food can be considered low compared to exposure from supplements, which are available at much higher doses due to the concentrated nature of supplements and shots.
8. The Committee highlighted that assumptions would have to be made on how many products, such as ginger shots, were consumed per day. The Committee noted that, as it is commonly understood that ginger suppresses morning sickness, it could not be ruled out that pregnant women would be using the supplements in this way. Diet plus supplement exposure would need to be considered, as well as diet plus shots depending on the exposure period of concern.
Consumption of ginger from food sources
9. The FSA Exposure team have sourced information on Ginger intake in women of childbearing age from food. Due to the limited information on consumption amounts of supplements and drinks in pregnant women, exposure was estimated based on the compositional information and usage information in widely available supplements and information on concentrated drinks. Full details of the ginger sources are given in Table 1 - 4.
Table 5: Estimated ginger exposures from a variety of sources in women aged 16 – 49 years old.
|
Source |
Range of daily exposures (g/day) |
Range of daily exposures (g/kg bw/day) |
Mean acute exposure* (g/day) |
Mean acute exposure* (g/kg bw/day) |
97.5th percentile acute exposure* (g/day) |
97.5th percentile acute exposure* (g/kg bw/day) |
Mean chronic exposure* (g/day) |
Mean chronic exposure* (g/kg bw/day) |
97.5th percentile chronic exposure* (g/day) |
97.5th percentile chronic exposure* g/kg bw/day |
|
Fooda |
No data. |
No data. |
1.7 |
0.026 |
11 |
0.16 |
0.55 |
0.0083 |
3.4 |
0.058 |
|
Drinks (Including tea and shots) b1,b |
0.5 - 32.5 |
0.0071 - 0.46 |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
|
Supplements c |
0.010 - 24 |
0.00014 - 0.34 |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
No data. |
1This assumes only one serving is consumed per day.
a Data obtained from the National Diet and Nutrition surveys years 1-8 calculated from women of a childbearing age (16-49 years) (Bates et al., 2014; 2016; Roberts et al., 2018).
b Data obtained online from retailers, see Appendix 1 for further details.
c Data obtained online from retailers, see Appendix 1 for further details.
*Rounded to 2 significant figures.
Table 5 provides exposure estimates for women of childbearing age - (16 - 49 years) 1 from years 1 – 8 of the NDNS survey (Bates et al., 2014; 2016; Roberts et al., 2018). The NDNS (Bates et al., 2014; 2016; Roberts et al., 2018) does not provide data for pregnant or lactating women so while data is based on women of childbearing age, this data may not necessarily be representative of the maternal diet. The food groups used for the exposure assessment consisted of all foods within the NDNS database which contained ginger (raw, powdered etc) except for alcoholic beverages. Mean acute ginger exposure from the diet of women aged 16-49 years old was 0.026 g/kg bw/day, and at a 97.5th percentile consumption was 0.16 g/kg bw/day. The corresponding mean and 97.5th percentile chronic exposure was 0.0083 and 0.058 g/kg bw/day. The upper value of the range of exposure from drinks and supplements was over double those estimated from 97.5th percentile acute consumption from food.
10. As the NDNS does not provide data for pregnant women, there would be uncertainty as to whether the data in Table 1 are an accurate reflection of consumption during pregnancy. This uncertainty also extends to data presented for drinks and supplements, as the patten of consumption during pregnancy to alleviate symptoms of sickness is unknown.
Further Information
Table 6: Ginger content in shots, teas and other drinks.
|
Shots |
Notes |
|
|
Contains 25% ginger in 110 ml shot, equivalent to 27.5 g fresh ginger. |
|
Innocent Shots Ginger Kick, Kicking Ginger & Spicy Turmeric 100ml |
Contains 10% ginger juice in 100 ml shot, equivalent to 10 g fresh ginger. |
|
Contains 2.5% ginger in 110 ml, equivalent to 2.75 g fresh ginger. |
|
|
Contains 26% organic ginger juice in 70 ml, equivalent to 18.2 g fresh ginger. |
|
|
Contains 40% organic ginger juice in 70 ml, equivalent to 28 g of fresh ginger. |
|
|
Contains 17.2 g of ginger in a 60 ml shot |
|
|
Contains 16% ginger juice in 60 ml shot, equivalent to 9.6 g of fresh ginger. |
|
|
Teas |
Notes |
|
Myrtle & Maude - Morning Sickness Herbal Tea - Peppermint & Ginger for Nausea Relief |
Contains 25% ginger in each tea bag. Assuming that each bag is approximately 2 g, they will contain 0.5 g of dried ginger. |
|
Pukka Lemon, Ginger and Manuka Honey 20 Herbal Tea Sachets 40g |
Each tea bag contains ginger root 32%. Assuming each bag is 2 g, they will contain 0.64 g of dried ginger. |
|
Each tea bag contains 37% ginger root. Assuming each bag is 2 g, they will contain 0.74 g of dried ginger. |
|
|
Contains 52% ginger root. For a 2 g tea bag, this is equivalent to1 g of dried ginger. |
|
|
Contains 70% ginger root. For a 2 g tea bag, this is equivalent to 1.4 g of dried ginger root. |
|
|
Contains 65% ginger. For a 2 g tea bag, this is equivalent to 1.3 g of dried ginger. |
|
|
Other drinks |
Notes |
|
Contains 2.2% ginger in 250 ml, equivalent to 5.5 g fresh ginger. |
|
|
Contains 11% fresh root ginger infusion and 2% pressed ginger juice in a 500 ml product. This is equivalent to 65 g fresh ginger and 32.5 g in a 250 ml serving. |
|
|
Contains 1% ginger juice in 330 ml, equivalent to 3.3 g of fresh ginger. |
Please note the different forms of ginger (i.e., gingerols, ginger extract, dried ginger root, fresh ginger) which may not be directly comparable.
Table 7: Consumption of ginger from supplements.
|
Supplement |
Maternal supplement? |
Form of ginger |
Recommended dose per person/day |
Daily Consumption (g/kg bw)* |
Notes |
|
Yes |
Ginger extract 10 mg |
0.010 g |
0.00014 |
No data. |
|
|
Yes |
Ginger root extract 58.5 mg |
0.05 9g |
0.00084 |
No data. |
|
|
No |
Dried ginger root 1.2 g |
1.2 g |
0.017 |
No data. |
|
|
Boots Pharmaceuticals DIGESTION SUPPORT TRAVEL with added Ginger 30 Capsules |
No |
Ginger Root Extract to 345 mg and Ginger root - 750 mg |
0.35 g extract + 0.75 g ginger root |
0.005 + 0.011 |
No data. |
|
Good n Natural Ginger Root Capsules 550mg | Holland & Barrett |
No |
Ginger root |
1.1 g |
0.016 |
2 capsules daily |
|
No |
Ginger extract |
6.0 g |
0.085 |
No data. |
|
|
No |
Ginger root powder + Ginger root extract |
0.15 g + 0.30 g |
0.0021 +
0.0043 |
No data. |
|
|
No |
Ginger root |
0.75 g |
0.011 |
No data. |
|
|
No |
Ginger root concentrate |
1.5 g |
0.021 |
No data. |
|
|
No |
24 mg gingerols equivalent to 14.4 g fresh ginger |
14.4 g |
0.20 |
No data. |
|
|
Ginger 12000mg x 120 Tablets | Nausea - Stomach Settler - Aids Digestion | Neulife Health & Fitness |
No |
Ginger extract 600 mg equivalent to 12 g fresh ginger- |
24 g |
0.34 |
1-2 capsules a day |
|
No |
Ginger Extract (equiv. herb powder 1000 mg) 50 mg |
2 g |
0.028 |
2 tablets/day |
*Consumption per body weight based on recommended dose rounded to 2 significant figures.
is calculated from the daily recommended intake and the average body weight of women aged 16- 49 years (70.3kg).
^Indicates whether the supplement is marketed specifically to pregnant or breastfeeding women.
Please note the different forms of ginger (i.e., gingerols, ginger extract, dried ginger root, fresh ginger) which may not be directly comparable.
References
Bates, B.; Lennox, A.; Prentice, A.; Bates, C.; Page, P.; Nicholson, S.; Swan, G. (2014) Available at: National Diet and Nutrition Survey Results from Years 1, 2, 3 and 4 (combined) of the Rolling Programme (2008/2009 – 2011/2012)
Bates, B.; Cox, L.; Nicholson, S.; Page, P.; Prentice, A.; Steer, T.; Swan, G. (2016) Available at: National Diet and Nutrition Survey Results from Years 5 and 6 (combined) of the Rolling Programme (2012/2013 – 2013/2014)
Roberts, C.; Steer, T.; Maplethorpe, N.; Cox, L.; Meadows, S.; Page, P.; Nicholson, S.; Swan, G. (2018) Available at: National Diet and Nutrition Survey Results from Years 7 and 8 (combined) of the Rolling Programme (2014/2015 – 2015/2016)