First draft statement on the safety of ginger supplement use in pregnancy
On this page
Skip the menu of subheadings on this page.This is a paper for discussion.
This does not represent the views of the Committee and should not be cited.
Introduction
1. As part of the current programme of work on the maternal diet, the Committee considered the use of dietary supplements during pregnancy. A scoping paper (TOX/2020/51) was presented, reviewing the commonly used dietary supplements during pregnancy. These were supplements that were not officially recommended by the relevant authorities, but which were promoted by anecdotal evidence and unofficial sources as having various purported benefits. The review was confined to herbal dietary supplements which would be regulated under food law, and which would not be considered to be traditional herbal medicines which are the responsibility of the Medicines and Healthcare Products Regulatory Agency (MHRA). Following this review, the COT agreed ginger required further investigation, noting that human, animal and in vitro data were available.
2. In May 2021, the Committee considered the potential effects of ginger and ginger supplements during pregnancy and lactation. Paper TOX/2021/26 (Available on the COT website) reviewed the available data on toxicity to the mother, effects on the development of the fetus or embryo, and possible interactions with drugs as well as data on potential exposure. The minutes discussing this paper are attached at Annex B to this paper
3. Overall, it was concluded that there were limited data. The human data presented were not strongly indicative of any toxicological concern but there were some indications of possible adverse effects and a lot of uncertainties. Ginger did not appear to be systemically toxic but did appear to have reprotoxic effects at high supplemental doses. The Committee suggested looking at the animal data in closer detail to determine the point of departure (No Observed Adverse Effect Level - NOAEL), followed by calculating the potential exposure to supplements to determine whether there was cause for concern.
4. Paper TOX/2021/51 provided further information with respect to animal studies, contaminants and exposure to ginger supplements, primarily centred on the effect of ginger on prostaglandins, reproductive and developmental toxicity and the possible contaminants present in ginger.
5. The members noted that although the different ginger extracts were not comparable, they did appear to exhibit some biological activity in the early stages of pregnancy. It was reiterated that there was no indication of general systemic toxicity from the use of ginger.
6. The current statement draws on the information provided in the previous discussion papers to form overall conclusions on the safety of the use of ginger and in particular ginger supplements in the maternal diet.
Questions for the Committee
i. Does the Committee have any comments on the structure and content of the statement?
ii. Does the committee have any further comments?
Secretariat
May 2022
TOX/2022/42 Annex A
Background
1. Ginger (Zingiber officinale) is a flowering tropical plant originating in Southeast Asia and grown in warm climates including China, India, Africa and the Caribbean. The rhizome (underground stem) of the ginger plant is commonly used as a spice and flavouring in many countries around the world and is increasingly growing in popularity as a natural remedy due to its purported immune system-boosting properties and also for motion sickness and post-operative nausea and vomiting.
Uses
2. Ginger is commonly consumed in fresh root form, dried root powder, capsule (encapsulated dried powder) form, liquid extract, preserved in syrup or sugar and as a tea. In pregnancy it is most used in the treatment of pregnancy-related nausea (NHS). It has also been used as a dietary supplement and a traditional remedy in many cultures. Ginger is included in the official pharmacopoeias of several western countries.
Constituents
3. Over 100 compounds have been identified in ginger extracts, the main being terpenoids - mainly sesquiterpenoids (α-zingiberene, β-sesquiphellandrene, β-bisabolene, α-farnesene, ar-curcumene (zingiberol) and smaller amounts of monoterpenoids (camphene, β-phellandrene, cineole, geraniol, curcumene, citral, terpineol, borneol) (EMA, 2012).
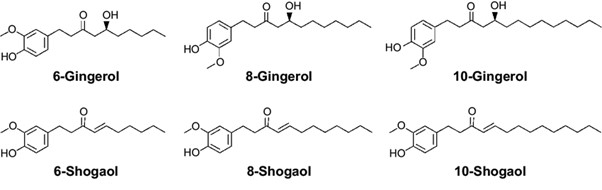
4. The ginger rhizome contains two main classes of constituents: the essential oils responsible for the aroma, and the main pungent principles, gingerols and shogaols. Organic acids are also present in smaller amounts. Depending on area of cultivation, gingerols make up 4-7.5% of the pungent principles, the main one being 6-gingerol. Gingerols of other chain lengths are also present in smaller amounts.
Reviews by other regulatory agencies
5. Ginger is included in the official pharmacopoeias of several western countries. Ginger is classified as ‘Generally Recognised as Safe’ (GRAS) by the United States Food and Drug Administration (FDA) however, few specific studies have been carried out to evaluate the safety of ginger use during pregnancy and lactation.
6. In 2008, the Danish company Ferrosan A/S withdrew their product GraviFrisk – a product containing 6 g of dried ground ginger - from market, due to concerns surrounding the lack of safety data with respect to the use of supplements containing highly concentrated ginger extracts by pregnant women (Dietz et al., 2016).
7. In their 2012 report on ginger root in powdered form, the European Medicines Agency (EMA) concluded “The ginger extract dosages to provoke acute toxicity are high and much higher than usually administered dosages (factor 10-15 for an adult). There is some evidence that ginger root may cause testicular weight to increase by repeated high dosages of ginger root extract (2000 mg/kg). Ginger root has mutagenic as well as antimutagenic properties in microbial test systems. Developmental toxicity studies in rats are difficult to interpret, however, it is probably not a cause for concern. In general, toxicity studies of ginger are considered inadequate at least regarding genotoxicity, carcinogenicity and, partially, reproductive and developmental toxicity.”
8. The Norwegian Food Safety Authority have issued a warning regarding the use of ginger supplements and ginger-containing shots during pregnancy. This was based on a risk assessment carried out by the Danish Technical University and the Danish Veterinary and Food Administration (DTU, 2018). The assessment, based on animal studies, including one where rats were treated with a fresh grated ginger preparation with ginger at concentrations of 20-50 g/L in water, found that even in the 20 g/L treatment group – the equivalent of 1784 mg/kg bw increased the incidence of abortion in rats. The Norwegian Food Safety Authority concluded that while a woman of 70 kg would consume less ginger (124 mg to 329 mg) there remains cause for concern and fetal risk cannot be excluded.
9. Recently, the Finnish Food Authority has issued a recommendation against the use of products containing ginger concentrate or extract, ginger tea and food supplements containing ginger by pregnant and breastfeeding women, infants and toddlers, schoolchildren, elderly and individuals with weakened immunity (Finnish Food Authority, 2019). It was noted that the concentrates contained harmful substances and safe consumption levels were unknown.
Health based guidance values
10. There are currently no health-based guidance values (HBGV) with respect to ginger or its main components. Exposure to ginger was considered based on information found on supplement and tincture composition and background diet, but the variability of available supplements meant exposure also varied, which made comparison difficult.
Toxicology
11. Paper TOX/2020/51 provided a detailed summary of the supplements most recommended during pregnancy (ginger, chamomile, raspberry leaf, echinacea, peppermint oil and leaves, dandelion, and evening primrose oil), focusing where available, on studies relevant to pregnancy and maternal outcomes. The main areas of investigation were general toxicity to the mother, effects on the development of the fetus or embryo, and possible interactions with medicines. Members suggested ginger required further investigation, noting that both human and animal in vitro and in vivo data were available.
12. Initially, the COT noted that intake of ginger in foodstuffs should also be considered as ginger was noted to be consumed not only as a supplement but also as part of the diet in foods such as ginger biscuits, tea and ginger beer. Therefore, aggregate exposures would need to be considered when addressing the safety of ginger supplement use during pregnancy.
13. It was noted that some studies detailed effects on male testes and, though not relevant for females, they were nevertheless regarded as indicating a potential reprotoxic effect from ginger. Studies suggest that ginger affected the viability of pregnancy; however, with no strong conclusive human data, the COT concluded that more work was required, especially as these studies suggested a link between first trimester loss and ginger use. Further, the possible fetotoxicity based on evidence from animal data, genotoxicity and possible drug interactions should be further investigated.
14. Discussion paper TOX/2021/26 reviewed the available studies on cytotoxicity, mutagenicity, acute, reproductive and developmental toxicity, lactation and possible drug interactions as well as data on potential exposure in pregnancy, covering both animal and human studies. Reports were shown to be varied due to the variability of forms and extracts tested and as a result, some findings were contradictory.
15. Paper TOX/2021/51 provided further information with respect to animal studies, contaminants and exposure to ginger supplements, primarily centred on the effect of ginger on prostaglandins, reproductive and developmental toxicity and the possible contaminants present in ginger. The Committee noted that the papers reviewed covered ginger in a range of forms including fresh, aqueous, dried and alcohol extracts.
Cytotoxicity
16. Ginger was demonstrated to exhibit cytotoxicity in some cases, with IC50 concentrations ranging from 9.08 µg/ml in human CCA cell line CL-6 (Plengsuriyakarn et al., 2012), to 39.2 μg/ml against breast (MCF7) and colon (LS174T) cell lines (Zaeoung et al., 2005). However, it was noted that the inhibitory concentration (IC50) values presented in the studies reviewed were based on a small amount of data, from only six different cell lines and therefore firm conclusions could not be drawn.
Toxicity in Animals
17. The animal studies on reproductive toxicity considered in TOX/2021/26 reported a number of findings, including reduced maternal weight gain, increased fetus weight, increased serum testosterone level in F1 generation males and an increase in embryonic loss.
18. The Committee considered the animal studies to be inconclusive however they noted that there were indications for a potential point of departure from available animal studies at around 50-100 mg/kg based on the reproductive studies considered.
19. ElMazoudy and Attia (2018) noted reductions in bodyweight and mortalities in mice dosed up to 2000 mg/kg bw/day and Alnaqeeb et al. (2003), observed increases in serum aspartate aminotransferase (AST) in female rats dosed up to 500 mg/kg. However, the Committee noted that the database was limited and on the basis of the available information, more data would be needed in order to allow for a robust investigation of the effects described above. Therefore, at present, the Committee were unable to determine a point of departure, to reach a conclusion.
Toxicity in humans
20. The COT considered a number of epidemiologic studies investigating the use of ginger during pregnancy (TOX/2021/26). For the most part, few studies explicitly addressed the safety of ginger consumption during pregnancy, as most were focused on the use of ginger as a treatment for nausea (Fischer-Rasmussen et al., 1990; Smith et al., 2004; Ensiyeh et al, 2009), age-related neurological disorders or pregnancy-induced sickness and therefore focused on efficacy (Willetts et al., 2003; Stanisiere et al., 2018). However, safety was considered in a few studies. The studies considered by the Committee included observational and randomised clinical studies, lasting from 4 days to 20 weeks in duration (Vutyavanich et al., 2001; Portnoi et al., 2003). Ginger in various forms were investigated in doses ranging from 750 mg/day to the equivalent of 7 g/day.
21. The study results in pregnant women were also varied and the overall findings inconclusive. Findings reported included abdominal discomfort, vomiting and diarrhoea. There were reports of an increased incidence of spontaneous abortion, but also some contradictory studies. There were no reported effects of defects post-partum following exposure to ginger.
22. The COT considered the mode of action of the purported benefits of ginger on nausea. It was theorised that ginger might decrease prostaglandin levels, which were linked to nausea.
23. The Committee noted the potential effect of ginger on the prostaglandin pathway, in particular Cyclooxygenase-1 (COX1) and Cyclooxygenase-2 (COX2) inhibition and how this may affect early pregnancy. One study examining the effects of ginger extracts on prostaglandin E2 (PGE2) production in vitro (Lantz et al 2007) demonstrated that crude organic extracts (dichloromethane-methanol, 1:1 v/v) of ginger were capable of inhibiting PGE2 production and that the compounds may act at several sites. The most potent effect on lipopolysaccharide (LPS) induced prostaglandin production was noted at less than 0.1 µg/ml. It was noted that the half maximal inhibitory concentration (IC50) values for a range of components were given, and it was demonstrated that the components mainly acted on COX-2. The COT concluded further studies would be needed to determine the role of increased prostaglandin levels in the early termination of pregnancy.
24. Overall, it was concluded that there were limited data. The human data presented were not strongly indicative of any toxicological concern but there were some indications of possible effects and a lot of uncertainties. Ginger did not appear to be systemically toxic but did appear to have reprotoxic effects at high supplemental doses.
Lactation
25. With respect to lactation, the focus of available studies has been on the effect of ginger on milk production and volume rather than safety and therefore, the effect of exposure during lactation has not been fully investigated.
Effect on Cytochrome P450 Enzymes and Herb-Drug Interactions
26. Cytochromes P450 are a family of isoenzymes responsible for the biotransformation of several drugs. Induction or inhibition of CYP enzymes is a major determinant of the occurrence of drug-drug interactions. In vitro studies indicated ginger extract and the major components thereof may have an inhibitory effect on CYP isoenzymes CYP3A4, CYP2C9 (Kimura et al., 2010) CYP2C19 (Kim et al., 2012) and CYP1A2 and CYP2C8 (Mukkavilli et al., 2014).
27. Several reports have been published on the pharmacological properties of ginger, with varying results. Human data showed possible interactions with medicines, including antibiotics, immunosuppressants, and anticoagulant medications (Okonta et al, 2008; Egashira et al., 2012; Rubin et al., 2019).
Anti-platelet aggregation activity
28. Ginger was reported to have antiplatelet activity (Srivastava, 1986,1989; Young et al., 2006), with some studies reporting effects in animals at doses of 500 mg/kg bw (Thomson et al., 2002). This further highlighted the need to differentiate exposure from the normal diet to that from supplements. Members noted that associations with haemorrhagic effects were reported following supplemental exposure to ginger, (Kruth et al., 2003; Rubin et al., 2019; Al Askar et al., 2020) though these were inconclusive.
29. A study by ElMazoudy and Attia (2018) linked follicular failure to haemorrhagic effects in a study investigating the effect of dried ginger root on the oestrus cycle and implantation, in female mice. The authors concluded that ginger impairs the normal growth of the corpus luteum because of progesterone insufficiency during early pregnancy and that the results suggested that ginger can disrupt the oestrous cycle and blastocyst implantation without teratogenesis. They considered the highest NOAEL to be 500 mg/kg bw. The COT noted that this might be worth further investigation. However, it was also noted that other factors could be contributing to the results observed and the study results were inconclusive.
Contaminants
30. Differences in cultivation conditions and extraction methods could lead to possible sources of contamination from microbiology, pesticides, heavy metals and residual solvents. Studies investigating contamination in ginger are limited, however of the few available, the main sources of contamination reported are heavy metals (Wagesho & Chandravanshi, 2015; Goroya et al, 2019, Kilic & Soylak, 2019; Xu et al, 2020) and mycotoxins (Ałtyn and Twarużek, 2020; Wen et al, 2014; Omotayo et al, 2019; Lippolis et al., 2017).
31. The Committee discussed the potential presence of contaminants in ginger and noting that the ginger products used in the studies reported were sourced locally in markets or herbalists (Wagesho & Chandravanshi, 2015; Goroya et al, 2019), Members queried whether there were any specific data on contaminants in ginger supplements available in the UK.
32. The Committee noted it was unknown how much ginger and particularly, highly concentrated juice extracts, would contribute to overall contaminant exposure in the UK.
Exposure
33. TOX/2021/26 discussed exposure to ginger via the diet and in supplement form. TOX/2020/51 examined in more detail exposure to ginger in the form of highly concentrated juices (‘shots’).
34. Many ginger supplements are recommended to support digestive and joint health, alleviate nausea, upset stomach, and travel sickness. Currently, two commercially available pregnancy supplements – ‘Seven Seas Pregnancy’ and ‘Seven Seas Pregnancy Plus Follow On’ – contain 10 mg ginger extract.
35. The availability of supplements in different forms, along with a lack of information with regards to extraction processes involved and therefore composition of the extracts, meant it was not possible to consider aggregate exposures, as such, ginger exposure from the diet and supplements were separately considered.
36. Mean acute ginger consumption from the diet of women aged 16-49 years old was 0.026 g/kg bw/day, and 97.5th percentile consumption was 0.16 g/kg bw/day. The corresponding mean and 97.5th percentile chronic consumption was 0.0083 and 0.058 g/kg bw/day, respectively. The upper value of the range of consumption from drinks and supplements was more than double (%) those estimated from 97.5th percentile acute consumption from the diet.
37. As the NDNS does not provide data for pregnant women, there was uncertainty as to whether the data presented was an accurate reflection of consumption during pregnancy. This uncertainty also extended to data presented for drinks and supplements, as the patten of consumption during pregnancy to alleviate symptoms of sickness is unknown.
Conclusions of the Committee
38. Ginger is commonly used as a spice and flavouring in many countries worldwide and is increasingly growing in popularity as a natural remedy, due to its purported immune system-boosting properties, for easing motion sickness and post-operative nausea and vomiting.
39. Several ginger supplements are commercially available, ranging from dried root in capsule form to tincture form, all with varying amounts of ginger. In addition to this, concentrated ginger shots, containing large amounts of pressed ginger, are increasingly becoming popular. The variability in the composition of these supplements adds uncertainty on the amount of ginger actually being consumed.
40. Study authors noted that some of the toxicity observed varied according to the nature of extraction solvent - organic solvent extracts exhibited more toxicity than aqueous extracts, which presumably indicates extraction of differentially toxic compounds. Hence, studies of individual extracts might not give the whole picture of the uncertainties involved.
41. Overall, the Committee concluded that based on the available information it was not possible to determine a point of departure to use in the risk assessment of ginger when used as a supplement.
42. Members noted that although the different ginger extracts were not comparable, there did appear to be some biological activity in the early stages of pregnancy. It was stressed that in general there was no indication of systemic toxicity from the use of ginger in the diet as food.
43. The lack of safety and toxicological information available on ginger use in pregnancy make it difficult to fully characterise the risks in this respect.
The committee noted that while there was some equivocal evidence for the possible effect of ginger on reproduction, it was not possible to characterise based on the data available.
44. Also, consumption data was based on women of childbearing age and therefore may not be representative of the maternal diet, leading to an under/overestimation of the actual exposure.
45. There is no clear indication that ginger is detrimental to pregnant women. Generally, normal levels of consumption of ginger within a diet is not considered a health concern. The Committee also noted that from the evidence presented, the potential for contamination of ginger with heavy metals and/or mycotoxins cannot be excluded.
COT Secretariat
July 2022
References
AlAskar, A; Shaheen, NA; Khan, AH; AlGhasham, N; Mendoza, MA; Matar, DB; Gmati, G; AlJeraisy, M; AlSuhaibani, A: (2020). Effect of daily ginger consumption on platelet aggregation. Journal of Herbal Medicine. Volume 20, 100316. https://doi.org/10.1016/j.hermed.2019.100316.
Alnaqeeb MA, Thomson M, Al-Qattan KK, Kamel F, Mustafa T, Ali M. (2003): Biochemical and histopathological toxicity of an aqueous extract of ginger. Kuwait J Sci Eng, 30: 35-48.
Al Omari, I; Afifi, F; Salhab, A. (2012). Therapeutic Effect and Possible Herb Drug Interactions of Ginger (Zingiber officinale Roscoe, Zingiberaceae) Crude Extract with Glibenclamide and Insulin. Pharmacognosy Communications. 2. 12-20. DOI:10.5530/pc.2012.1.4.
Ałtyn, I., & Twarużek, M. (2020). Mycotoxin Contamination Concerns of Herbs and Medicinal Plants. Toxins, 12(3), 182. https://doi.org/10.3390/toxins12030182The Committee on Toxicity of Chemicals in Food, Consumer Products and the environment (COT) (2020). Scoping Paper on Herbal Supplements Used in Pregnancy.
The Committee on Toxicity of Chemicals in Food, Consumer Products and the environment (COT) (2021). The potential effects that ginger and ginger supplements may have during pregnancy and lactation.
DTU Food Institute, (2018). The safety of pregnant women when ingesting ginger shots made from the root from real ginger (Zingiber officinale Roscoe).
Dietz, Birgit & Hajirahimkhan, Atieh & Dunlap, Tareisha & Bolton, Judy. (2016). Botanicals and Their Bioactive Phytochemicals for Women's Health. Pharmacological reviews. 68. 1026-1073. Doi:10.1124/pr.115.010843.
Egashira, K; Sasaki, H; Higuchi, S; Ieiri, I (2012). Food-drug Interaction of Tacrolimus with Pomelo, Ginger, and Turmeric Juice in Rats, Drug Metabolism and Pharmacokinetics, Vol 27, 2, 242-247. https://doi.org/10.2133/dmpk.DMPK-11-RG-105ElMazoudy, Reda & Attia, Azza. (2018). Phytomedicine. 50. 2018, 300-308, Ginger causes subfertility and abortifacient in mice by targeting both estrous cycle and blastocyst implantation without teratogenesis.
Ensiyeh, J.; Sakineh, M.A. (2009). Comparing ginger and vitamin b6 for the treatment of nausea and vomiting in pregnancy: A randomised controlled trial. Midwifery 2009, 25, 649–653. https://doi.org/10.1016/j.midw.2007.10.013
European Medicines Agency (2012): Assessment report on Zingiber Officinale Roscoe, rhizome; EMA/HMPC/577856/2010.
Finnish Food Authority, (2019). General Instructions on Safe Use of Foodstuffs.
Fischer-Rasmussen, W.; Kjaer, S.K.; Dahl, C.; Asping, U. (1991). Ginger treatment of hyperemesis gravidarum. Eur. J. Obstet. Gynecol. Reprod. Biol. 1991, 38, 19–24. https://doi.org/10.1016/0028-2243(91)90202-v.
Krüth P, Brosi E, Fux R, Mörike K, Gleiter CH (2004). Ginger-associated over anticoagulation by phenprocoumon. Ann Pharmacother. Feb;38(2):257-60. doi: 10.1345/aph.1D225.
Getaneh, A., Guadie, A., & Tefera, M. (2021). Levels of heavy metals in ginger (Zingiber officinale Roscoe) from selected districts of Central Gondar Zone, Ethiopia and associated health risk. Heliyon, 7(4), e06924. https://doi.org/10.1016/j.heliyon.2021.e06924
Goroya K, Mitiku Z, Asresahegn Y, (2019). Determination of concentration of heavy metals in ginger using flame atomic absorption spectroscopy. Afr. J. Plant Sci. 13, 163–167. DOI: 10.5897/AJPS2019.1787.
Kilic S, Soylak M (2020). J Food Sci Technol 57, 927–933 (2020). Determination of trace element contaminants in herbal teas using ICP-MS by different sample preparation method.
Lippolis V, Irurhe O, Porricelli, ACR, Cortese M, Schena R, Imafidon T, Oluwadun A, Pascale M (2017). Natural co-occurrence of aflatoxins and ochratoxin A in ginger (Zingiber officinale) from Nigeria. Food Control 2017, 73, 1061–1067.
Mukkavilli, R., Gundala, S. R., Yang, C., Donthamsetty, S., Cantuaria, G., Jadhav, G. R., Vangala, S., Reid, M. D., & Aneja, R. (2014). Modulation of cytochrome P450 metabolism and transport across intestinal epithelial barrier by ginger biophenolics. PloS one, 9(9), e108386. https://doi.org/10.1371/journal.pone.0108386Okonta JM, Uboh M, Obonga WO. (2008). Herb-drug interaction: a case study of effect of ginger on the pharmacokinetic of metronidazole in rabbit. Indian J Pharm Sci. 2008 Mar-Apr;70(2):230-2. doi: 10.4103/0250-474X.41462. PMID: 20046719; PMCID: PMC2792472.
Omotayo, O. P., Omotayo, A. O., Babalola, O. O., & Mwanza, M. (2019). Comparative study of aflatoxin contamination of winter and summer ginger from the North West Province of South Africa. Toxicology reports, 6, 489–495. https://doi.org/10.1016/j.toxrep.2019.05.011
Plengsuriyakarn, T.; Viyanant, V.; Eursitthichai, V.; Tesana, S.; Chaijaroenkul, W.; Itharat, A.; Na-Bangchang, K. (2012). Cytotoxicity, Toxicity, and Anticancer Activity of Zingiber Officinale Roscoe Against Cholangiocarcinoma, Asian Pacific Organization for Cancer Prevention, 13(9), pp. 4597–4606. doi: 10.7314/apjcp.2012.13.9.4597.
Portnoi, G., Chng, L. A., Karimi-Tabesh, L., Koren, G., Tan, M. P., & Einarson, A. (2003). Prospective comparative study of the safety and effectiveness of ginger for the treatment of nausea and vomiting in pregnancy. American Journal of Obstetrics and Gynecology, 189(5), 1374–1377. https://doi.org/10.1067/s0002-9378(03)00649-5
Rubin D, Patel V, Dietrich E. (2019). Effects of Oral Ginger Supplementation on the INR. Case Rep Med. Jun 11; 2019:8784029. doi:10.1155/2019/8784029. PMID: 31281366; PMCID: PMC6594244.
Smith, C; Crowther, C; Willson, K; Hotham, N; McMillian, V. (2004). A Randomized Controlled Trial of Ginger to Treat Nausea and Vomiting in Pregnancy. Obstetrics and Gynecology. 103. 639-45. DOI:10.1097/01.AOG.0000118307.19798.ec.
Srivastava KC (1986). Isolation and effects of some ginger components of platelet aggregation and eicosanoid biosynthesis. Prostaglandins Leukot Med. Dec;25(2-3): 187-98. doi: 10.1016/0262-1746(86)90065-x. PMID: 3103137.
Srivastava KC (1989). Effect of onion and ginger consumption on platelet thromboxane production in humans. Prostaglandins Leukot Essent Fatty Acids. Mar; 35(3):183-5. doi: 10.1016/0952-3278(89)90122-1 PMID: 2710801.
Stanisiere, J., Mousset, P. Y., & Lafay, S. (2018). How Safe Is Ginger Rhizome for Decreasing Nausea and Vomiting in Women during Early Pregnancy? Foods (Basel, Switzerland), 7(4), 50. https://doi.org/10.3390/foods7040050
Thomson M, Al-Qattan KK, Al-Sawan SM, Alnaqeeb MA, Khan I, Ali M (2002). The use of ginger (Zingiber officinale Rosc.) as a potential anti-inflammatory and antithrombotic agent. Prostaglandins Leukot Essent Fatty Acids. Dec; 67(6):475-8. DOI: 10.1054/plef.2002.0441. PMID: 12468270.
Tiran, D. (2012). Ginger to reduce nausea and vomiting during pregnancy: Evidence
of effectiveness is not the same as proof of safety. Complementary Therapies in Clinical Practice 18 (2012) 22-25.
Vutyavanich T, Kraisarin T, Ruangsri R. (2001). Ginger for nausea and vomiting in pregnancy: randomized, double-masked, placebo-controlled trial. Obstet Gynecol. 2001 Apr;97(4): 577-82. DOI: 10.1016/s0029-7844(00)01228-x. PMID: 11275030.
Wagesho Y, Chandravanshi BS, (2015). Levels of essential and non-essential metals in ginger (Zingiber officinale) cultivated in Ethiopia. SpringerPlus 4, 1–13. Doi: https://doi.org/10.1186/s40064-015-0899-5
Wen J, Kong W, Hu Y, Wang J, Yang M (2014). Multi-Mycotoxins analysis in ginger and related products by UHPLC-FLR detection and LC-MS/MS confirmation. Food Control 2014, 43, 82–87. doi: 10.1016/j.foodcont.2014.02.038.
Willetts KE, Ekangaki A, Eden JA. (2003). Effect of a ginger extract on pregnancy-induced nausea: a randomised controlled trial. Aust N Z J Obstet Gynaecol. 2003 Apr;43(2):139-44. doi: 10.1046/j.0004-8666.2003.00039.x. PMID: 14712970.
Xu J, Zhang J, Lv Y, Xu K, Lu S, Xiaohui Liu, Yang Y, (2020). Effect of soil mercury pollution on ginger (Zingiber officinale Roscoe): Growth, product quality, health risks and silicon mitigation. Ecotoxicology and Environmental Safety, Volume 195, 2020, 110472, ISSN 0147-6513. https://doi.org/10.1016/j.ecoenv.2020.110472
Young HY, Liao JC, Chang YS, Luo YL, Lu MC, Peng WH (2006). Synergistic effect of ginger and nifedipine on human platelet aggregation: a study in hypertensive patients and normal volunteers. The American Journal of Chinese Medicine. 34(4):545-551. DOI: 10.1142/s0192415x06004089
Zaeoung, S.; Plubrukarn, A.; Keawpradub, N. (2005) Cytotoxic and free radical scavenging activities of zingiberaceous rhizomes. Songklanakarin J. Sci. Technol. 2005, 27, 799–812.
Annex B TOX/2022/42
The Final minutes of the meeting of the Committee on 4th May 2021 can be accessed COT Meeting: 4th May 2021 | Committee on Toxicity (food.gov.uk)